For some people their inflammatory bowel disease (IBD) requires that they need surgery to manage their condition. For some surgery is needed in an emergency, life-saving situation but for most it can be planned ahead.
It’s estimated that around 70% of people with Crohn’s disease and 25% of people with ulcerative colitis (UC) will need surgery during their life to help treat their IBD. Surgery is less common in people who have microscopic colitis.
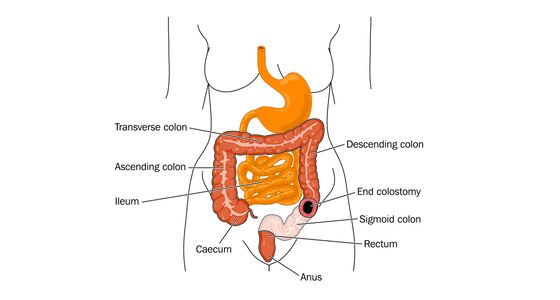
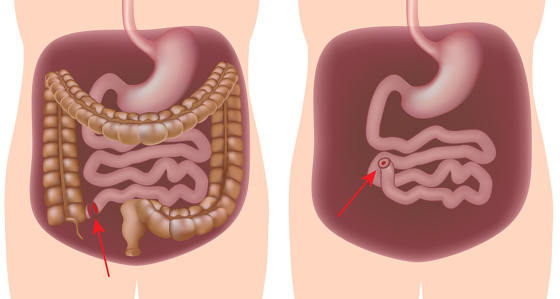
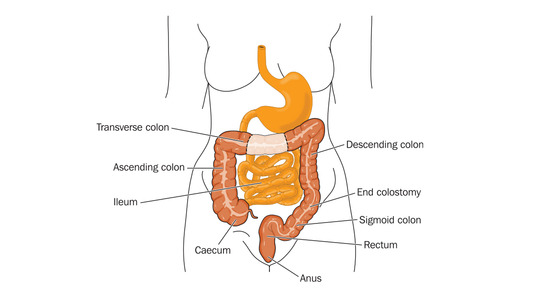
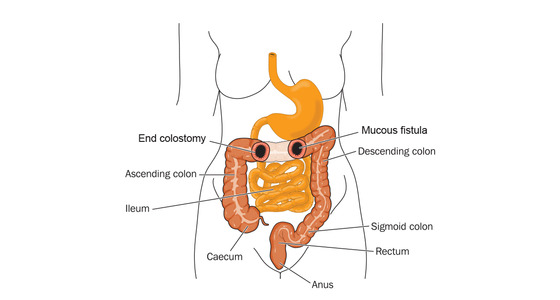
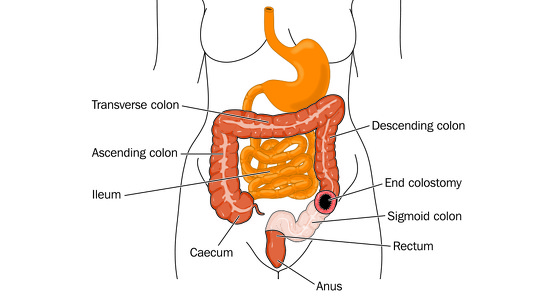
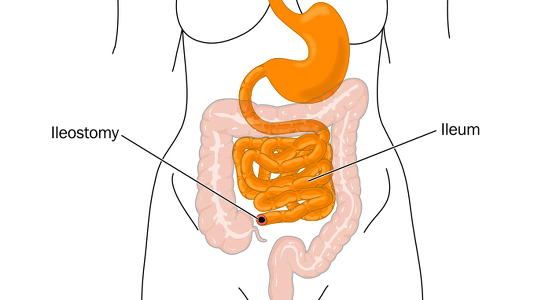
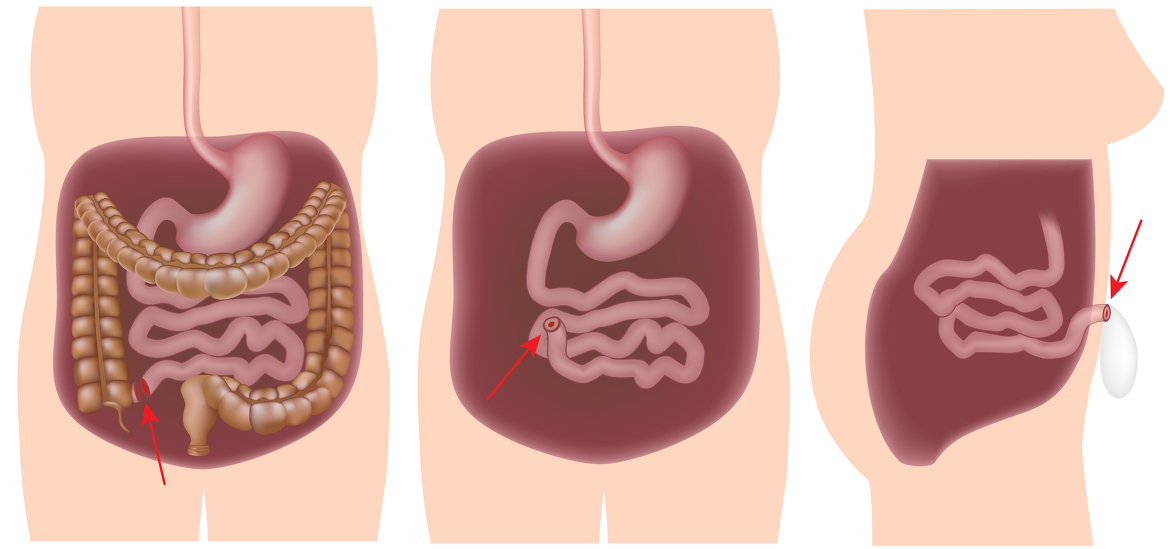
In general, surgery for IBD removes part the part of the bowel (large or small intestine) which is damaged and/or inflamed or treats strictures (narrowing) or abscesses or fistulas. In some cases surgery can mean a stoma is created on the surface on your stomach and your bowel waste goes into a bag, in others the bowel is reconnected. The type of surgery, though, varies from person to person depending on the type of IBD you have and the severity of any damage to your bowel.
Before opting for surgery it is important to understand what the aim of the surgery is, what will happen during the procedure, the recovery period needed and take into account any other considerations. It is also helpful to understand about how the digestive system works and where your IBD is so that you can see what the surgery is trying to achieve.
IBD is a lifelong, chronic condition and having surgery to remove diseased parts of your gut does not cure you, though it may remove some or all of your symptoms. There is also a risk that the inflammation will return to parts of the gut which remain. If you have UC and have all of your large bowel, rectum and anus removed then there is no risk of inflammation returning (however you may still experience symptoms such as fatigue, joint pain).
The reasons for surgery vary from person-to-person. In extreme cases a person is rushed to hospital and the surgery takes place with little notice - in others you have time to consider the surgery and decide if it’s for you.
Some of the reasons people opt for surgery include:
It is estimated that around 7 in 10 people with Crohn’s disease receive surgery at some point in their life.
The most common operations for Crohn’s disease include:
Around one in four people with UC receive surgery at some time during their life.
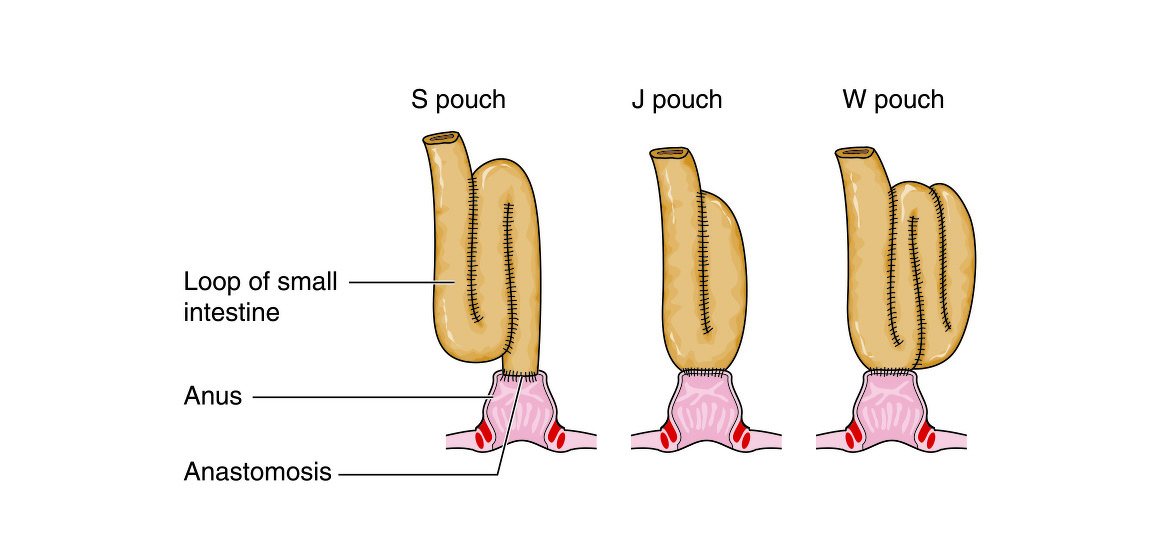
The most common operations for UC include:
If you have ulcerative colitis and have all of your colon, rectum and anus removed then there is no risk of the inflammation returning (as there is nowhere colon for it to return to!), however you may still suffer from other IBD symptoms such as fatigue and joint pain.
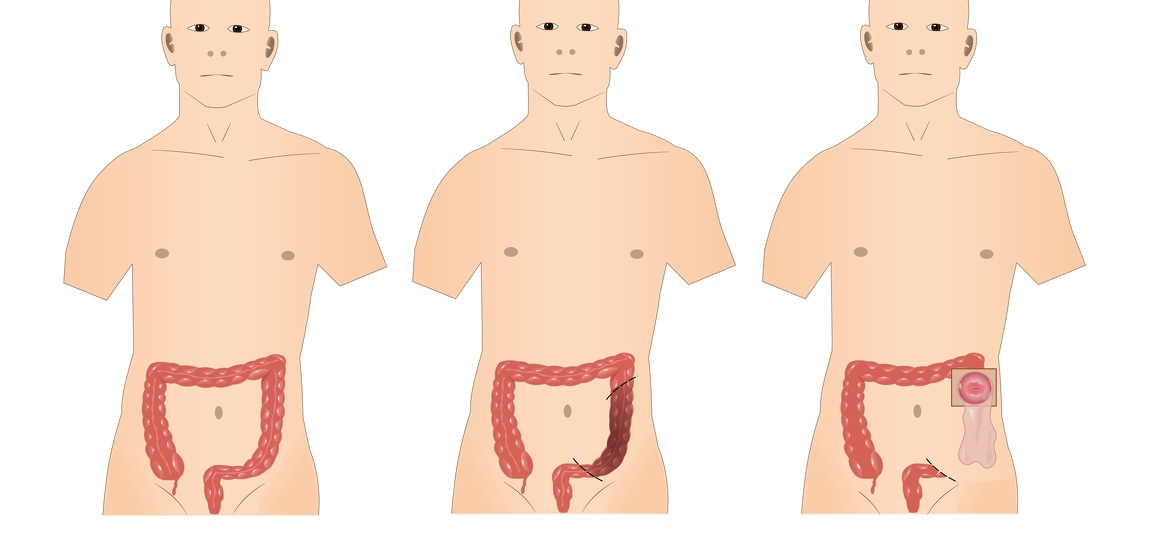

Many of the procedures can now be carried out through keyhole surgery (laparoscopy). This is where several small incisions are made rather than one large one.
As mentioned earlier, a stoma is where the end of the bowel it brought to the surface of the abdomen and waste passes out through it into a bag, rather than through the rectum.
Stomas may be either permanent or temporary depending on the type of surgery you have had.
As with any surgical procedure there are risks which need to be weighed up against the pros of having the surgery. The risks vary, depending on the type of surgery you are having and your own personal circumstances.