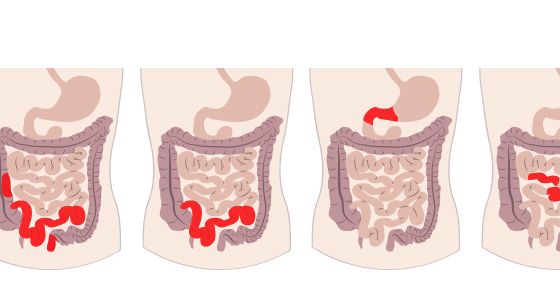
For many people with inflammatory bowel disease (IBD) - Crohn’s disease, ulcerative colitis or microscopic colitis - diarrhoea is a normal, everyday occurrence. It is one of the most common symptoms for most types of IBD. The diarrhoea is often mixed with blood, or mucous and pus.
If you are experiencing this type of diarrhoea for the first time then it can be understandably distressing. It’s important that if you see any blood in your stool, or the frequency of your toilet trips does not improve, that you seek medical advice.
Diarrhoea in people with IBD is often accompanied with urgency to use the toilet which cannot be easily controlled. This can sometimes result in ‘accidents’ where people soil themselves.
Sometimes, periods of diarrhoea can be mixed with periods of constipation where you are unable to pass stools. This will often be accompanied by abdominal pain.
Despite receiving treatment for their IBD some people still unfortunately suffer from diarrhoea of varying degrees and they have to find ways to cope with it in their everyday life.
Diarrhoea is the frequent passing of loose, watery stools. It is also often accompanied with urgency to use the toilet which cannot be controlled and can lead to bowel incontinence.
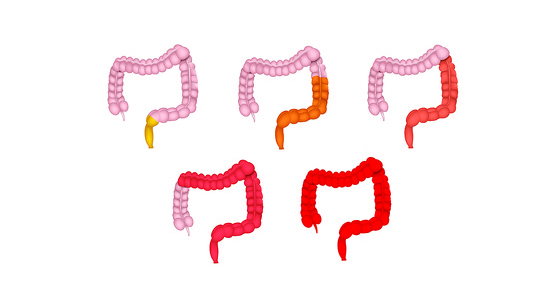
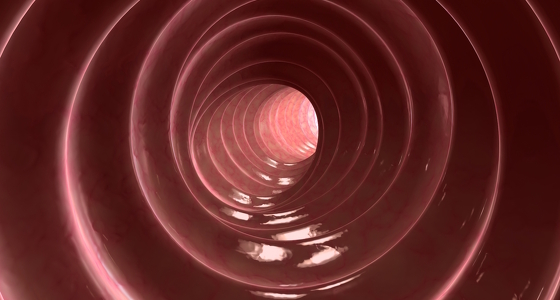
Diarrhoea happens when the large colon is unable to absorb all of the water from the waste passing through it. In people with some types of IBD the colon often becomes ulcerated and inflamed during a ‘flare’, making it difficult for water to be absorbed. Because the stools are very watery they move more quickly through the colon - causing the urgency and frequency associated with diarrhoea.
Diarrhoea often happens in people with IBD who are having a ‘flare’ but there may be other reasons for watery stools too. These include:
There is often blood mixed with the diarrhoea due to the ulcers that form in active IBD on the surface of the gastrointestinal tract. These ulcers have a tendency to bleed. The damaged intestinal lining can also produce mucous which may also be seen in the diarrhoea.
Diet
You may have food sensitivities which could cause diarrhoea. Common sensitivities include dairy, gluten, some fruits and vegetables - keep a food diary to see if there are any food ‘triggers’ for your diarrhoea
Greasy/fatty foods, caffeine, gassy (carbonated) drinks and alcohol can cause diarrhoea.
Try eating smaller portions of food more frequently so that your bowel has less food to process
Medication for IBD
There are many medications available for IBD which aim to get your disease under control and then into remission - and therefore reducing the diarrhoea you experience. These medications have different effectiveness for different people. You can read more about them in our section on medication.
Antidiarrhoeal drugs - such as Loperamide
These work to slow down the contractions in the gut which push food through - thus slowing down bowel movements. The patient advice leaflets which come with these medications advise against taking them if you have IBD as they can cause serious side effects, including toxic megacolon. If you are thinking about taking antidiarrhoeal drugs you should discuss this with your doctor first.
Antispasmodic drugs - such as Buscopan and Colofac
These relax the intestinal muscles to slow down bowel movements. These are generally safe to take with IBD but check with your doctor before taking them.
Bile salt drugs
If you have diarrhoea as a result of bile salt malabsorption (BAM) then bile salt drugs can be given to help with this. BAM is fairly common in people with Crohn's disease that affects the ileum but is often undiagnosed.
Bulk formers
These are granules made from plant fibre which when taken swell up inside the bowel. They both thicken loose stools and soften hard stools. They are generally safe for people with IBD but shouldn’t be taken in some situations - such as if you have a stricture - so always check with your doctor first.
If you are suffering from diarrhoea you will be losing a lot of fluid as well as electrolytes therefore it’s important that you are replacing these. You can buy electrolyte tablets and solutions to assist with this.
Many people who continue to suffer with diarrhoea as a result of their IBD go through periods of ‘remission’, where their diarrhoea may be less frequent, and others when they are in a ‘flare’ and their diarrhoea is more frequent.
There are many people who find ways to cope with the diarrhoea by making some adaptations so that they can live a fairly normal life.
The key is often to spend some time working out if there is anything which causes your diarrhoea to get worse and then some ways of dealing with it. At first this can seem like an impossible task. But, if you keep a diary you may find that some patterns do start to emerge. Unfortunately the ‘triggers’ are different for everyone so you will need to discover these for yourself. At first try noting down when you are going to the toilet against what you have recently eaten, what you have recently been doing etc. Some people find there are certain foods - such as dairy, gluten, certain fruits and vegetables - which make their diarrhoea worse. They also find that certain environmental factors - such as a stressful situation or anxiety at work - may play a part. There are some apps available to buy which can help you to keep track of these things.
Once you have started to identify these you can work out ways to avoid - or minimise - contact with any ‘triggers’. You may find it useful to take a look at our diet survey to give you an idea of what foods other people with IBD have found can be ‘triggers’. If you think you have a sensitivity to a whole food group such as dairy it is important to discuss this with a dietician to ensure you are getting all the nutrients you need.
Many people with IBD keep a ‘caught short kit’ which has essential items they may need if they aren’t able to make it to a toilet in time and need to clean themselves up. These homemade kits often include spare clothing, wet wipes, bin bags, soap, anal barrier cream. Another useful item to carry is a Radar key (disabled access toilet key). How these are governed varies from country to country. In the UK these can be bought online or are issued by some councils and disabled associations.