There are various medications which may be given to people with inflammatory bowel disease (IBD) to try to control their symptoms and get them into remission. They fall into four main categories:
Which medication (and even which brand) you are given will depend on the type of Crohn’s disease, ulcerative colitis or microscopic colitis you have, your IBD symptoms and the response you have had to any other medication you have taken.
Your doctor will assess all of these factors, alongside disease treatment pathways to make decisions about your medication.
Some medications are used to induce remission (get you better), some are used as maintenance treatment (to keep you well) and some are used for both. You can find out more about induction and maintenance treatments here.
You may also be prescribed two or more medications to take at the same time. This is known as combination therapy.
When you have IBD it's likely you will need to take medicines long-term, possibly for the rest of your life, so it's important that you get into a good routine for managing your medications to make sure you always have a good supply and know what medicines you take and when.
The following is provided as information only.

Aminosalicylates are usually the first medicines prescribed to people newly diagnosed with IBD. They may be given as tablets, liquid, creams or suppositories to people with mild to moderate ulcerative colitis and mild Crohn’s disease to induce or maintain remission. They may be taken orally or via your back passage. Aminosalicylates are usually more effective for people with ulcerative colitis than with Crohn’s disease, but the effectiveness varies greatly from person to person.
The medicine works to reduce inflammation in the gut, although the exact way it works is not fully understood. Aminosalicylates contain 5-aminosalicylic acid (5-ASA).
Types of aminosalicylates - or 5-ASAs - include:
There may also be some other brands available not mentioned above.
As with all medications some people may experience side effects. Common side effects include headache, nausea, abdominal pain and cramping, loss of appetite, vomiting, rash, or fever. 5-ASA agents can also cause diarrhoea in a small number of users, though it can be difficult to distinguish if the diarrhoea is as a result of the medication or from your IBD.
Rarely aminosalicylates can cause problems with your blood and you should tell your doctor immediately if you have any unexplained bleeding, bruising, red or purple discolourations of the skin, sore throat, high temperature (fever) or if you feel generally unwell during treatment. You should discuss potential side effects with your doctor before taking the medication and read the patient information leaflet which comes with the medication.
They should not be used by people with known kidney problems.
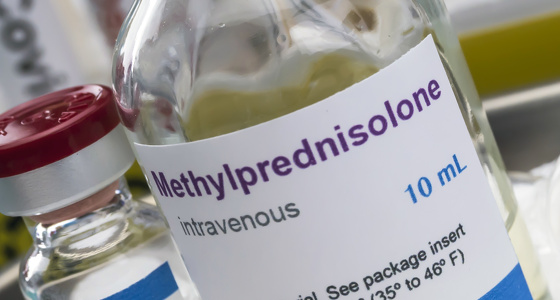
Corticosteroids work to reduce inflammation for people with all forms of IBD - Crohn’s disease, ulcerative colitis and microscopic colitis. They are also immunosuppressive - meaning they suppress the immune system. As a result some people find they are more susceptible to catching infections.
Corticosteriods are often given if aminosalicylates have not been effective. They are powerful and fast-acting and help to reduce symptoms quickly, often within days. They are used as an induction therapy, so once you are in ‘remission’ (where you don't have inflammation or symptoms) your doctor will slowly reduce your dose of corticosteriods until you no longer take them.
They may be given as tablets, liquid, creams or suppositories to be taken orally, via your back passage or as topical creams. For some people, with severe cases of IBD, they may be given corticosteroids intravenously into their vein (usually done in hospital).
Types of corticosteroids include:
There may also be some other brands available not mentioned above.
Corticosteroids should not be used long-term as they can have undesirable side effects. Side effects include round of the face (known as moon face), weight gain, acne, osteoporosis, insomnia and mood swings.



Immunomodulator medicines weaken or suppress the immune system. This decreases the inflammatory response the body has which is thought to play a role in IBD flares.
They are used as a maintenance therapy to keep you well. Azathioprine and 6-Mercaptopurine are both also used in the treatment of fistulas. They are taken orally as tablets, although some forms can also be applied topically or given as injections.
Types of immunomodulators include:
Azathioprine, methotrexate and mercaptopurine can take between 3-6 months to work so may be combined with another medication, such as corticosteroids, initially.
As immunomodulators suppress the immune system you may be susceptible to catching infections more easily. They can also have an effect on bone marrow, liver and kidneys, therefore you may be required to have regular blood tests to check these.
As with all medications some people experience side effects. The reported side effects vary depending on the type of immunomodulator taken. You should discuss what these side effects are with your doctor before taking the medication.
Biologics are genetically engineered from living organisms and target specific proteins and enzymes in your body that cause inflammation. They are more targeted than some other medications used for IBD which suppress the whole immune system.
Different types of biologics target different proteins and enzymes thought to play a role in IBD. The targets include tumor necrosis factor (TNF)-alpha, interleukins, adhesion molecules and colony-stimulating factors.
Biologics are the newest medication to be used to treat Crohn’s disease and ulcerative colitis and can be used as both an induction and maintenance treatment.
Types of biologics include:
How the biologic is given, and the frequency at which it is given, depends on the type of biologic your doctor thinks is best for you.
Infliximab, natalizumab and vedolizumab are all given via intravenous infusions, usually in a hospital or at a medical centre.
Adalimumab, certolizumab pegol, cimzia, ustekinumab and golimumab are given by injection. Some patients may be able to inject themselves at home.
Biosimilars are imitations of biologic drugs which have already been registered for use. In recent years the number of biosimilar medicines has increased and you may be given a biosimlar instead of one of the brands listed above. Biosimilars are not identical to the biologic they are imitating, but are very similar.
Side effects of biologics may include: headache, fever, chills, difficulty breathing, low blood pressure, and hives. Additionally, patients may experience stomach pain, back pain, rash, nausea, and upper respiratory infection (cough and sore throat).
You should discuss potential side effects with your doctor before taking the medication and read the patient information leaflet which comes with the medication.
The new small molecule medications approved for use in IBD are possible treatment options for adults with moderately or severely active ulcerative colitis when other treatments have been tried but prove unsuccessful. This means, in general, if your ulcerative colitis did not respond adequately to standard treatments or biologic treatments, you have not got better or have stopped getting better while on them, or you can’t tolerate standard treatments, biologic treatments and the side effects. Small molecule drugs are compounds that regulate or modify a biological process. They are used as an anti-inflammatory medicine that modifies the immune system but in a different way to biologics. They affect the immune system by blocking the ability of lymphocytes (white blood cells) to escape from the lymph nodes into the gut, where they can cause inflammation. They achieve this by sticking to the lymphocytes which stops them travelling through the gut mucosa, the innermost layer of the gastrointestinal tract.
The next generation of small molecule medications block enzymes involved in activating your body's immune system, reducing inflammation. They are known as Janus kinase (JAK) inhibitors. The JAK inhibitor medications used in treating ulcerative colitis are:
Other new small molecule medications belong to a class of medicines called sphingosine 1-phosphate (S1P) receptor modulators. The sphingosine 1-phosphate (S1P) receptor modulator used in treating ulcerative colitis is:
Different small molecule medications have the potential for different side effects. More details about the specific side effects for each medication are available in the following articles…
As well as the medications above you may also be given some medications to help with other symptoms you experience as a result of your IBD.
Antacids
Antacids work to control acid levels in your stomach for people who suffer from heartburn, acid reflux and indigestion.
Read more about antacids and who can't take antacids.
Proton-pump inhibitors
PPIs are used to reduce gastric acid production and include omeprazol, esomeprazole, lansoprazole, pantoprazoleand rabeprazole. They are commonly used to treat acid reflux and ulcers of the stomach and part of the small intestine called the duodenum.
Pain relief
Unfortunately for some people with IBD pain is an everyday occurrence and can severely affect your quality of life. There are a range of pain relief options which you may be given, depending on the what and where the pain is. These include:
Before taking any medication please speak to your doctor as there are some medications which are not advised be taken if you have IBD (such as ibuprofen) or if you are already taking other medication.
Antibiotics
You may be given antibiotics if you are found to have an infection (such as Clostridium difficile (C. diff)), an abscess or fistula. For some people they are also given for the specific treatment of IBD.
Read more about antibiotics.




