If you have an anal fistula then it’s likely you will need treatment of some kind as they rarely go away by themselves. This article explores the different treatments available.
If you have an anal fistula then it’s likely you will need treatment of some kind as they rarely go away by themselves. The treatment you have will depend on the cause of your fistula, its location and whether it is a simple or complex fistula.
Often surgery is needed, carried out under general anaesthetic (being put to sleep), to heal the fistula. The goal of anal fistula surgery is to repair the fistula without damaging the surrounding anal sphincter muscles. These muscles are used to hold poo in your rectum and damage to them can cause faecal incontinence (being unable to hold your poo in).
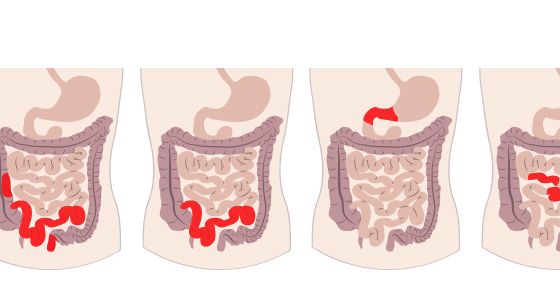
If your anal fistula is as a result of inflammatory bowel disease (IBD), such as Crohn’s disease, then you may be offered medication, surgery, or a combination of both to treat it and try to prevent more fistulas occurring in the future. Up to a third of people with Crohn’s disease who have a fistula will need surgery at some point.
This is a commonly used surgery to treat anal fistulas. In this procedure the fistula is cut lengthways, opened up and cleaned, allowing it to heal as a flat scar. The healing process can take anywhere from a week to several months. This operative is often done as a day case, meaning you won’t need to stay in hospital overnight.
It is an effective treatment, but if the fistula passes through more than a small amount of the anal sphincter muscles another treatment might be more suitable to reduce the risk of incontinence caused by damage to the muscle.
A seton is a piece of thread (surgical thread) that is passed through the external hole of the fistula, along the tunnel of the fistula and then out through the internal opening. It is this brought down through the anus (bottom) and tied in place to form a loop. It is left in place for several weeks. This stops the fistula from closing and allows any fluid (such as infection from an abscess) to drain away.
A seton is often used if the fistula passes through a large amount of anal sphincter. It is usually inserted under general anaesthetic and the external fistula hole covered with a dressing to absorb the fluid that drains from it. This dress will need to be regularly changed and the area kept clean. You will be shown how to do this.
To get the fistula to heal completely you may need to have the seton replaced with a tighter one, or have some surgery.
In the case of people with Crohn’s disease a seton will likely be used in conjunction with a medication such as infliximab or with another surgical procedure.
If your anal fistula passes through anal sphincter muscles then a fistulotomy may not be suitable. If this is the case an advancement flap procedure may be suggested. In an advancement flap procedure the fistula is cut or scraped out. The internal opening of the fistula is then covered using a piece of skin or tissue taken from the anus or rectum
Although this has a lower success rate than a fistulotomy, it avoids the need to cut the anal sphincter muscles which can cause incontinence (losing control of your bowels).
In this procedure a cone-shaped plug is used to block the internal opening of the fistula. Over time new tissue grows where the plug is to heal the fistula. The external opening is left open so that the fistula can drain. The plug is made from animal tissue.
The plug is usually inserted under general anaesthetic
The procedure can come with some complications, including pain, an abscess forming or the plug being pushed out of place.
In a fistulectomy the fistula is completely cut out. It is usually carried out under general anaesthetic as a day case (meaning you don’t stay in hospital overnight).
A fistulectomy is considered to be more effective than a fistulotomy, however the recovery time can be longer and there is a higher risk of complications, such as damage to the anal sphincter.
In a LIFT procedure the surgeon makes a small cut in the skin above the fistula. Through this cut the fistula tunnel is then cut into two sections and each end is stitched closed.
This is a fairly new technique.
A small camera is used to see inside the fistula tract. It is cleaned out and then sealed using an electric current. Sometimes stitches or fibrin glue are used instead. VAAFT is a good way to identify if there is more than just one fistula tract or any abscesses present.
In this non-surgical procedure done under general anaesthetic fibrin glue is injected into the fistula. This seals it and helps it to heal. Although not as effective as a fistulotomy, it can be a good option if your fistula goes through anal sphincter muscles.
If the fistulas are as a result of an infection from an abscess then you may be given antibiotics to help, however often surgery is also needed to heal the fistula.
If the fistula/s is as a result of Crohn’s disease (fistulizing Crohn’s disease) then often a combination of medication and surgery is required. This is to both treat any fistulas and also try to get inflammation under control to prevent more fistulas in the future.
Some of the medications that may be used in these cases are:
Antibiotics - metronidazole, ciprofloxacin
These may be used to clear any infection related to the fistula or abscess. They may help to heal the fistula, however recurrence rates are high. Combining an antibiotic and a biologic medication or immunomodulator (such as azathioprine) may have more success1.
Biologic medications - anti-TNFs (infliximab, adalimumab), ustekinumab, vedolizumab
Anti-TNFs may be used to help with fistula drainage and support fistula closure in people who have Crohn’s disease. One study looking at infliximab was found to provide a 50% or more reduction in fistula drainage in 68% of patients and complete fistula healing was seen in 55% of patients2.
It has been found that people who had a combination of both infliximab and surgery saw their fistula heal quicker and had a longer time to relapse in the case of complex fistulas than those who had just surgery or used infliximab alone3.
If anti-TNFs are not effective then treatment with another biologic, such as ustekinumab or vedolizumab may be used.
Thiopurines - Azathioprine, 6-mercaptopurine
Thiopurines, such as a azathioprine or 6-mercaptopurine (6-MP), may be used to treat perianal fistulas in people with Crohn’s disease. Studies have shown that thiopurines can provide clinical improvements in some patients4.
Other medications that may be used - ciclosporin tacrolimus, methotrexate, thalidomide
References
Other resources used
https://www.guysandstthomas.nhs.uk/health-information/anal-fistula-treatment/surgery
https://www.nhs.uk/conditions/anal-fistula/treatment/
https://www.nhs.uk/conditions/anal-fistula/treatment/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4316082/
https://academic.oup.com/ecco-jcc/article/14/8/1049/5699755
https://www.crohnscolitisfoundation.org/what-is-crohns-disease/treatment/surgery/fistula-removal
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155133/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4040755/