Name: Alwine Jarvis
Year of Birth 1958
Lives: Essex, UK
Type of IBD: Ulcerative colitis
Details of Surgery: Restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) - aka J-pouch
After around 30 years of living with ulcerative colitis I took the decision in 2015 to have a restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA), also known as J-pouch, surgery. In layman’s terms this is the removal of your large bowel and rectum, preserving the anal sphincter and just leaving a rectal cuff of, in my case 1cm, to attach the J-Pouch to. In the first of my two operations the surgeon also creates a J-pouch laparoscopically, as well as a temporary ileostomy. The second operation reverses the ileostomy and connects the J-pouch so one can use a toilet again in the normal way.
My latest flare started in March 2014 and by June 2015 it had got progressively worse, to the point where I often had accidents after leaving home. None of the conventional medication managed to bring my ulcerative colits under control. Since February I had also been injecting Humira (Adalimumab) fortnightly, sadly my inflammation markers were still increasing month on month. That, coupled with my family history of bowel cancer, led me to make the decision to opt for elective surgery. My latest colonoscopy result in May stated that the crypt abscesses in my bowel were severe.
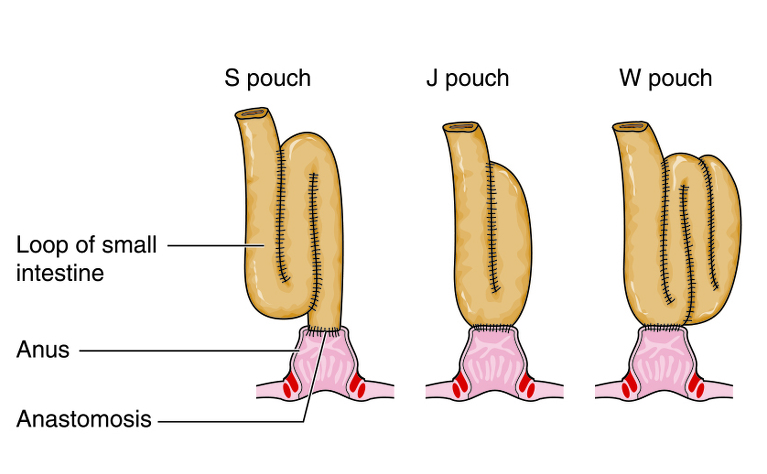
The J-pouch operation was my preferred choice, but because I’d had some other surgeries I required an examination on the operation day to see if I was a suitable candidate. The other option was a colectomy with permanent ileostomy.
The surgery was booked for July 6, 2015, and the week before flew by, especially as we were at a wedding in Cornwall from Thursday to Sunday. I had to start changing my diet by the Saturday and take some high carbohydrate drinks in preparation for the operation. These drinks are meant to help your recovery after surgery.
On July 6 I arrived at 7am at the hospital. The paperwork I was given stated 1st floor Elective Surgery, but they had moved the ward to the ground floor overnight and the doors were still locked with a padlock no one had a key to. It was quite stressful for the staff and obviously the patients, but I was lucky to be allocated a single room. The surgeon and his whole team came to see me and I was given the ok by the surgeon for the J-pouch operation, but I would not know until I woke up whether all had gone to plan.
The operation lasted five-and-a-half hours and I have no recollection of having been in post-op! My bed was by the nurses’ station and the surgeon came to see me that evening and said that visually my colon was in a far worse state than the colonoscopy in May showed and that it was the right decision to have opted for my colon to be removed.
A few days later the histology report confirmed that I actually had pancolitis, with deep crypt abscesses and I had been at risk of a perforated bowel. Thank God no dysplasia or cancer was detected and having had my colon removed, the risk of future bowel cancer has been eliminated. I was advised before my operation there is a very tiny chance I could get cuffitis or cancer in my rectal stump.
The next morning, at around 9am, the physiotherapists arrived to get me out of bed and walking. I had only got back to the ward about 6pm the previous night. I thought they were joking! The level of pain was intense, but I had a button I could press which gave me pain relief in the form of morphine. The first few days after surgery were difficult. I felt sick, nauseous, could not eat and the bowel had not woken up. The ileostomy bag was also a bit of a shock initially, mainly because the output was very, very watery and therefore I encountered many bag leakages which impacted on my confidence, but I knew it should get better and I was not afraid to cope with the stoma. I also had a catheter and when it was removed I was unable to pass urine and I went into retention. After a scan they replaced the catheter again for a further two days. For quite some time afterwards I could only pass urine with the tap running!
I was a bit unlucky as my stoma was very, very close to the skin. Usually it should have a good spout on it, but mine did not. I had leaks - the skin around my stoma became inflamed to the point of it bleeding. Initially it was an emotional struggle to change the bag, cope with the smell and just getting to grips with looking after myself. I was in hospital for eight days, mainly due to the bowel having gone to sleep for a few days. I was walking around by day two and wearing my FitBit to do as many steps as I could to help with the wind pain. I came home on July 14. I was making progress and a district nurse come to see me as the wound where one of the drains was placed was still severely leaking. Usually this dries up before people are released from hospital.
Sadly on July 19 I developed a blockage, which was serious. I was bringing up my own faeces and there was no output in my bag. I was so, so scared and felt extremely poorly. Eventually they managed to place an NG-tube up my nose and down my throat into my stomach, which immediately made me feel better, although the tube itself was uncomfortable, as it was irritating my throat. The blockage cleared after a few days and I was let home again. This knocked my confidence as I was scared of eating in case this happened again! I had lost about 19lbs (8.6kg) in the operation.
I slowly built up my confidence again and had support from my stoma nurses and the Crohn’s and Colitis Forum on Facebook, where I made some great friends! Sadly I encountered another blockage, in two places this time. It was six weeks later and I got admitted again via a phone consultation with my stoma nurse. I will always be grateful for her acting so swiftly. Again, I had been ill all night, walking about, trying to drink fluids in order to help clear the blockage despite feeling and being sick, much as before. The pain was bad with severe cramps, yet my bag remained empty! The X-ray confirmed my bowel was extended in two places, but worse in the lower right hand quadrant. Again I had to have an NG-tube. The process of placing the tube through my nose into my stomach was much easier on this occasion, possibly because I knew it would make me feel better. My bowel had well and truly gone to sleep, so it was ‘nil by mouth’ and just sips of water. Everything else was given via IV.
My veins are quite difficult to insert a line into, so they needed the help from the MEA team (Medical Emergency Assistance) to be able to give me fluids, painkillers and anti-sickness medication. My hospital stay lasted six days this time and I was discharged on September 8, 2015. I was sent home on a liquid/mushy food only diet, because my reversal operation was scheduled for September 29. My colorectal surgeon did not have any spare capacity to move my reversal date forward and I was advised by him, that he would first do an examination under anaesthetic (EUA) to deal with the two blockages, before then attempting the reversal operation. They did say I could have the blockages addressed sooner, but then my reversal operation would need to be rescheduled for some time in 2016, as the bowel needs time to recover from the past three months and the two operations. I chose to have the EUA and reversal at the same time.
I arrived on the day of my reversal operation to find out I was 3rd on the operating list. It could be a long day! However, my surgeon changed the list and I was second, for which I was grateful. Whilst waiting to go to theatre a doctor tried three times to get blood off me as they needed to do a cross match, in case I needed a blood transfusion. It was too late now, so the anaesthetist had to do this, but even he had difficulty getting the blood and placing the line in for the anaesthetic to be administered.
I woke up in post-op, this time fully awake and aware of my surroundings, and after another 90 minutes, once my blood pressure picked up a bit, I was transferred back to the colorectal ward. This surgery coupled with the EUA lasted two-and-half hours.
The next day I was euphoric! I felt so well, I was allowed to start eating a low residue diet and I could not have wished for more. It felt strange to use the toilet in a normal way again. I was told I could go home in two days if I continued to make good progress.
The following day everything changed! Overnight my bowel went to sleep again and I was placed on ‘nil by mouth’. The feeling of nausea and sickness was terrible and I got no relief from it at all. I was awake at night and felt extremely poorly 24/7. Sadly this lasted for the next five days! I felt so ill I wanted no visitors as I felt unable to talk to anyone. Then the bowel seemed to finally wake up and for the first time I felt like eating again. I had some toast with butter and I managed to keep it down. I was so pleased!
I was, however, a bit shocked they let me home the very next day, before I even had eaten a solid meal and the meal had passed through my new plumbing system. I was extremely nervous as I was so scared of encountering another blockage. I am pleased to report that I was fine though!
I had great support from my wonderful Enhanced Recovery Nurse who rang me daily at home for the next few days to see how I was doing. I also had a dedicated J-pouch nurse who I could ring if I needed any advice. She contacted me a few times as well and this really helped me feel less alone. I also joined ‘The J-Pouch Group’ on Facebook. The people on this forum were a great help to me! I listened to their advice and I have made steady progress. Three months post takedown I was now able to eat some fruit and vegetables, although I am still very limited with regards to what I can tolerate. I still can’t have fizzy drinks, cream, butter, cheese and normal milk just in moderation, as these increase my output tremendously. I know everyone is different and I also have to make allowances for having no gallbladder which is an additional hindrance, as I cannot absorb fat well.
My biggest problem after the reversal operation was the pain in my lower right hand quadrant (Right Iliac Fossa Pain ‐ RIF), which seemed to get worse over time and was in the exact place where previously the worst blockage was located. As I began to do more and started being more active the pain would increase. There was no rhyme or reason for it, especially as I had the EUA whereby the surgeon removed scar tissue from both blockages before starting the takedown operation. After I was home for five days I was asked to attend the surgical assessment unit at the hospital again to investigate the pain. However, all they did was take my blood and a urine sample. They said it is post-operative pain and it would get better. I received no ultrasound or other investigation. This unsettled me as I am quite a strong person, but due to my two previous blockages I was naturally nervous.
I had an appointment with my original Gastroenterologist (who referred me for surgery) and he arranged an urgent ultrasound scan for me. The scan showed no collection of fluid, but it detected the bowel was still extended in the same two places, where the previous blockages were, however, it was still within the given tolerances so there was no cause for concern.
I did and still do have at times a strong burning sensation of the skin around the anus. This is completely normal, but can be avoided by watching what foods cause this and also using products which will calm the skin down. A hot bath helps incredibly and when it is very severe I cut a 100% cotton handkerchief in four and place it between my bum cheeks. The relief is enormous! I also ordered Calmoseptine Ointment from Amazon as well as Bio Oil and Vicks Vaporub, yes really! They all help me with the burning sensation and the Bio Oil is also good for keeping scars moist.
I found my J-pouch nurse extremely helpful. I would ring her and knew she would get back to me. She always gave me good advice and put my mind at rest.
I saw my colorectal surgeon in mid-December, after returning from our first holiday since May the day before. We had been unable to travel before this time because of the severity of my UC and the surgeries. The consultant immediately commented on how well I looked, which was also seconded by my friends and family over the Christmas period. The RIF pain finally went away during this holiday in Germany, where we walked every day for at least five miles. To me this was a miracle as the pain had woken me without fail every single night and was troublesome during the day too. It was an intermittent, sharp, burning sensation that would take your breath away and in the early days I was unable to get out of bed fast enough to make it to the bathroom! At night I wore full Tena briefs, which prevented accidents and having to change the bed. Initially the night time frequency and the early evenings after the main meal were difficult, however, now everything has settled down, I am physically and mentally in a much better place!
I was advised by my surgeon to take Imodium as and when required and Codeine at night to help me sleep. In the mornings, I now take one Omeprazole to help line my stomach and a vitamin B complex as well as Metamucil (Physillium husks to help thicken my output) , which I personally have found very beneficial. I have managed to cut my Imodium intake to maximum 1 a day and have tried to cut out the Codeine. I am sure over time I will manage this, but it is still early days for me. On average I now go to the toilet 6 to 8 times a day, more often when I introduce new foods, eat sugary items or fatty foods, like cheese for instance. Over the past four weeks I have slept through the night three times, which has been a breakthrough. Prior to my reversal operation I had to get up to empty my stoma bag at least once during the night.
Would I do it all again? Of course, no question at all, I just wished I had done it years ago! I feel I have got my life back and I intend to make the most of my new J-pouch and get back to a very active and hopefully healthy life!
Remember this is my journey and I have written this in good faith to give potential J-pouchers an insight into how it was for me. This does not mean that your experience will be the same!
If anyone has any specific questions, or just wants to talk to me, you can contact me via IBDrelief.

