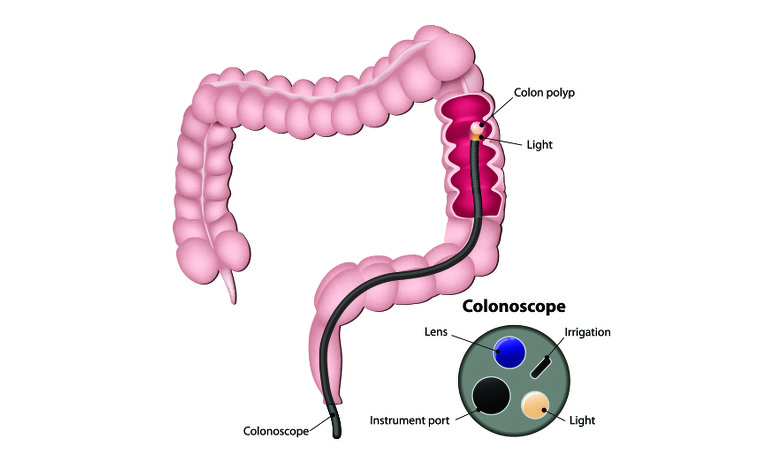
A colonoscopy is a type of endoscopy test which is carried out on the colon (large intestine).
A colonoscopy is a flexible tube with a light and telescopic camera at one end and is often referred to as a colonoscope. It is carefully inserted into your anus and images from inside your colon are transferred onto a screen for your doctor to view.
You may be given a colonoscopy if you are experiencing inflammatory bowel disease (IBD)-type symptoms as part of the diagnosis process and also as part of ongoing monitoring of your condition.
To aid with diagnosis a colonoscopy will be done when ulcerative colitis or Crohn’s disease are suspected.
Colonoscopies may also be carried out as part of the ongoing monitoring of your IBD to check inflammation levels and any signs of bowel cancer. People with IBD in their colon can be at a slightly higher risk of developing this type of cancer.
If you have IBD in your colon then you should have regular colonoscopies to monitor the inflammation and the extent of your disease and to also check for any signs of bowel cancer. Your doctor will advise you on how often it is necessary for you to have a colonoscopy.
A colonoscopy is usually carried out in hospital by a specially trained doctor or nurse. Unless you are already staying at hospital you will probably be seen as a day-case, meaning you do not need to stay overnight. Sedatives are sometimes used during the procedure so it’s important to have someone who can collect you from the hospital and to avoid driving for 24 hours after the procedure.
The procedure should take no more than an hour to carry out. You may receive a sedative or local anaesthetic before the test starts to make the examination more comfortable for you. This will be discussed with you before the examination.
You will be asked to lie on your left-hand side and the colonoscope will be carefully fed through your anus and all the way through your colon. It is long enough to also go into the end of the small intestine (known as the terminal ileum). A lubricant will be used to make this as easy as possible. As the colonoscope is passed through your colon you may need to move position or the doctor/nurse may press on your abdomen. This is to help the passage of the colonoscope and to get the clearest pictures possible.
During the procedure biopsies may be taken to be examined and polyps (small growths) may be removed.
After the procedure the doctor or nurse may discuss some of the findings with you, or you may be given a follow-up appointment. If biopsies have been taken then the results of these may not be available for several weeks. The results will be sent back to your doctor/consultant who can discuss them with you.
Once the effects of any sedative or anaesthetic have passed you should be able to go home the same day. You should arrange for someone to pick you up from the hospital and to stay with you for 24 hours to ensure all the effects of the medication have passed. During this time you may not be as coordinated as usual and be sleepy. You shouldn’t drive, drink alcohol, operate heavy machinery or sign any important documents.
If you are having a colonoscopy to aid diagnosis then the doctor or nurse will be looking at the lining of your colon and rectum (large bowel) to see if there are any signs for Crohn’s disease or ulcerative colitis. They will also check for signs of bowel cancer or other conditions which may be causing your symptoms.
If you have already been diagnosed with IBD then the colonoscopy will be used to check and monitor the extent and level of inflammation in your large bowel.
Different people have different experiences of colonoscopies. Some people report they find it very uncomfortable, while others sleep through it. Sedatives and/or local anaesthetics will be discussed with you before the procedure starts. Let the person carrying out the colonoscopy know if you are nervous about it or experience pain or discomfort during the examination.
Your doctor or nurse will advise you on exactly how they want you to prepare, but an outline of what to expect is given below.
The colon needs to be clear for the images from the colonoscope to be clear. Therefore, you may be asked to follow a specific diet and take strong laxatives (bowel prep) in the day or so leading up to the examination. The laxatives will give you diarrhoea so you may want to make sure you are able to stay close to a toilet during this time. You should continue to drink clear fluids (such as water or squash) to prevent yourself from getting dehydrated as a result of the diarrhoea.
The laxative is often provided as a liquid for you to drink at home and some people do not like the taste.
You may be asked to stop taking some medication - such as warfarin, aspirin or clopidogrel - as well as painkillers such as ibuprofen and iron tablets.
Preparing your colon ready for the examination can be unpleasant and time-consuming, however it is necessary to ensure the intestinal lining can be viewed clearly. If your bowel isn’t completely clear, and the colonoscopist isn’t able to see your full bowel during the procedure, then you may have to come back for another colonoscopy.
Colonoscopies are generally very safe procedures, but there is an extremely small risk of bowel perforation during the examination by the colonoscope or other instruments. You may want to discuss the risk with the physician performing the test.
Immediately afterwards you may feel bloated or uncomfortable and you may bleed a little from your back passage if you have had any biopsies taken. These side effects should pass quickly.
After returning home you should go to hospital straightaway if you experience bleeding from you back passage, have a swollen abdomen or pain that gets worse, feel weak or develop a fever.