In January 2014 I met a doctor from the IBD team. By now I had just finished my second round of steroids (I had tapered down to 20mg around Christmas but the symptoms came back with a bang so they upped me back up to 30mg again and I had tapered down again and was now off them - goodbye moon face!). I had also been really fortunate to visit Rome for 3 days for my birthday - yes I was exhausted and spent a lot of time on the loo and slept very well each night but my god Rome is a beautiful place and I am so glad I went.
So, at the back end of January I arrive at Hull Royal for my appointment, on my own - in hindsight not a great idea as I totally freaked out at one point - which I’ll tell you more about later. My advice is, take someone with you to your appointments for emotional support more than anything else.
I went into the doctor’s office, went through some of the usual questions - how are you now? What are your bowel movements like? (if you’re still not used to talking so openly about your bowel movements yet, you will be don’t worry) and then the doctor just stopped talking and was reading the notes on the screen over and over again. I asked if everything was ok and he said he was just reading the notes from my colonoscopy and MRI. With that he then said he needed to get a second opinion and was going to get the consultant, Dr S, and he left me on my own for a good 10-15 minutes. What did I do? Read the notes on the screen about my MRI which made no sense to me but sounded really scary. The words were probably scary as I didn’t know what they meant and also being left on my own for such a long space of time was also really terrifying, what were they saying? Why was it taking so long? Am I going to be getting out of here today? Am I wearing the right underwear for an overnight stay?! Dramatic thoughts, but this was me now freaking out!
The Dr and my new consultant Dr S (who I now have a long-standing Dr-patient relationship with as I see him every few months) returned and I was bracing myself for the news - I need an ostomy bag. My biggest fear I had at the time, seems really pitiful now as I have read so many stories of people who have such a better quality of life with having stomas, but I was only just coming to terms with being diagnosed, let alone having to adapt life with a bag.
No bag was mentioned but the question Dr S did ask me was; “What would you rather live with, the pain or the frequency of having to go to the toilet?”. At the time I thought it was a trick question, so he asked me again and to really think about my answer and the life that I lead. The answer was then really apparent to me; I couldn’t keep living with the pain, the sleepless nights, the stabbing agony on my right side, the constant dull back pain, the out-of-body experience I was going to experience in the next few days (we’re coming onto this).
I explained my set-up, working from home and having great flexibility in my life, that I could cope with frequency but the pain was something I couldn’t compromise with.
He then broke the news, he was referring me to a surgeon as I had a severely blocked terminal ileum brought on from the constant ulcerating and scarring. It was that bad no medication would make it better and was that badly diseased it needed cutting out. Cue my first obvious question: “Does that mean I need a bag?”. Dr S. explained he couldn’t say yes or no whether I would need a bag, it would all depend on how the surgery went - but a high proportion of these surgeries resulted in healthy anastomosis (the joining of the 2 ends of bowel together) so wouldn't require a bag.
They would open me up via keyhole and cut away 20cm of my small bowel, the terminal ileum valve, and a portion of my large bowel and then reconnect the two ends together. That’s why Dr S asked me about the frequency, as the valve between the two bowels acts as gateway, allowing motions through as and when required and I wouldn’t have that anymore so I was likely to need to use the toilet more than a normal person with a healthy bowel (nothing new there anyway) and there may be sudden rushes to use the toilet (again what’s new?!).
I remember the news sinking in and exhaling really loudly and I asked when - expecting to be on a hospital list for three months at least. Dr S replied as soon as possible. He was going to call the surgeon today and his team would be in touch to get an appointment sorted. To help things, and stop any further pain, I was to go onto a no fibre diet immediately, eat small meals and pick up some “Ensure” drinks from the pharmacy and have four a day to keep my nutrients up in my body. Dr S made sure I had the contact numbers for my IBD helpline and said if I had any other questions to give them a call and that I would see him again in three months post-operation.
I left the hospital feeling numb, cold, scared, shocked, in disbelief but weirdly pleased in some ways. For a while now I was starting to think that everything was in my head, the constant need for the toilet wasn’t an actual problem, the exhaustion was just laziness but this confirmed it all, this was actually serious and I was ill. Actually poorly enough I needed to have surgery - this was big!
This day was a Thursday and as I drove home I started to make some of the calls I needed to make - mum and dad, my brothers and my boss. Matt, my boss, was great and said he had been doing some research on Crohn’s as he knew nothing about it and had read that most people require surgery at some point, I was to just keep him informed of dates and how I was feeling with travel etc.
The next day, Friday, the surgeon secretary rings say she’s been asked to make a pre-surgery appointment with Mr G and could I make the following Tuesday to meet the surgeon, which I was not going to miss and booked it in.
Monday night, the night before my appointment, I had the worst pain ever. I was up from about 2am rolling around on the sofa passing in and out of consciousness with this intense cramping pain that would come and go in waves. If you’ve ever seen the Alien movies and the scene where the baby alien pops out of the guy’s chest over breakfast, that was the kind of frequency these waves were coming at - pulsing movements, something trying to force its way through the impossible and the pain being that strong it was knocking me between what felt like sleep and being awake. The pain finally subsided by 6am and I drifted back off to sleep.
I arrived at the hospital for the appointment and called in to see the surgeon and a nurse was present too. Mr G asked the same kind of routine questions, drew me a picture of what he was going to do (he was also going to whip out my appendix whilst he was in there, his word “whip” like the everyday occurrence it is to him) and with that I told him about the pain the previous night and he explained that it sounded like a blockage. This pain the night before confirmed for him how soon it needed to happen and I remember this memory so clearly; he picked up his phone, dialled a number, picked up a piece of paper that had times with names next to them. When the other person picked up the phone (his secretary) his words were, “I need to make a change to Thursday scrub off Mr XX and put in Simon Booth instead - case number XXXX for a ileocaecal valve removal” and he hung the phone up. My words were, “Which Thursday are you talking about?” to which he replied, “The day after tomorrow, that Thursday, we need to get you in as soon as possible”.
So that was that I was going in the day after next. To say I was shocked, stunned, discombobulated (love this word) are all understatements. Mr G asked if I had any questions, which I don’t think I did as I was too shocked and with that I was off to have my bloods taken and swabs for MRSA. His receptionist faxed over a letter for me detailing the time and place I needed to be and I was on my way home.
Cue planning mode for going into hospital for potentially a week depending on how I recovered. Mr G told me that they practiced an advanced recovery procedure where the day after my surgery they would move me out of bed for a few hours, the next day they’d get me walking a little bit and try keep me as mobile as possible as this enabled quicker recoveries. But it was still likely to be up to a week.
I got home, phoned work and was told to take the next few days off to get myself ready for what was to come. Rang my family and they were as surprised as I was. I needed to get a handover ready for work so my colleagues could pick up my workload as I was going to be off for up to four weeks minimum and go out and buy things like PJs/loungewear. I even Googled what to take into hospital with me as I had no idea what was common practice! Thank goodness for Google!
The night before my operation I actually went out to the theatre. We thought it would be a good idea to keep me busy and my mind off the next day. We watched Bouncers which was really good and I ate some chocolate - I didn’t have to fast beforehand which I thought was bizarre and didn’t have to take any prep either, which again was a surprise as I thought they would want me clean inside!
The Thursday morning arrived. I was up early as I needed to be at the hospital for 8am admission.
I arrived at the hospital, was admitted, weighed, blood pressure taken, gowned up (they are as bad as you think, nobody looks good in a gown and you’re totally aware your bum is probably sticking out), signed paperwork, met the anesthetist, met my surgeon’s team who asked if I had any last questions and then I sat”¦.and waited”¦..and waited some more. I was listening to some music, a song called To Build a Home by The Cinematic Orchestra (I’d heard it on a TV advert and purposefully chose this song as I find it really relaxing). With that a trolley turned up, with no one on it and a nurse mouthing something at me. I stop my music for her to say, “It’s time to go Simon”.
It’s time to face my biggest fear that I’ve not mentioned yet - being anaesthetised. This will be my first time and it’s always been something that I’ve been afraid of for a few reasons:
1. I’ve never had it before so it’s the fear of the unknown
2. What if I didn’t wake up?!
3. I hated the idea that someone was watching me “go under” and I had no control over it!
All of a sudden I felt my temperature drop as I was wheeled through to pre-op and the anesthetist’s assistant must have noticed as he got me a blanket and told me to relax and that he would be back for me soon. The waiting around was the worst part as you just don't know when it is time and everyone walks around in their normal environment doing their normal things and for me it was so alien.
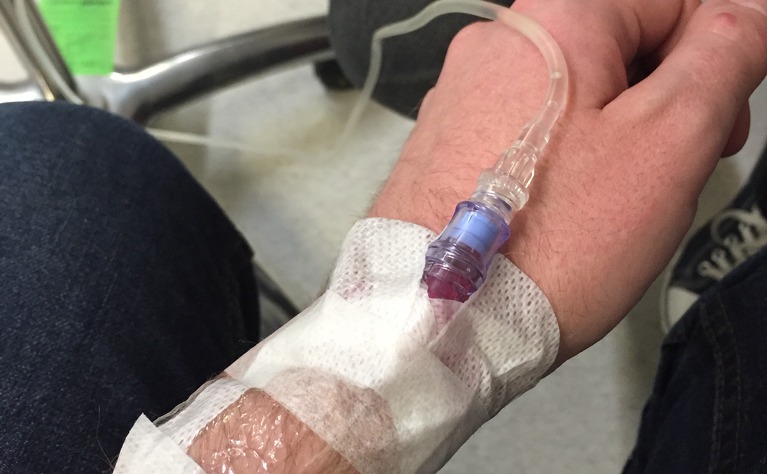
I’m eventually wheeled through to the anesthetic room and a trainee anesthetist struggles to get a cannula in my arm. I’m not sure if it’s his inexperience or that fact that my veins are just not playing ball. He eventually is successful and with that the assistant is back and explains I am having a temporary spinal block that will last 24 hours. This is to make the first day after surgery a bit more bearable on my abdomen seeing as they are going to be in there removing part of my bowel. I’m not sure if this is available to everyone but I found it really useful the next day. I’m sat on the edge of the bed having a very cold spray on the bottom of my back, a local anesthetic and then the spinal block, which automatically makes me lose the function of my legs, so the anaesthetist (who I met earlier) and the assistant (the trainee has been sent out) help me lay back down.
Time to face my fear! The time to go to sleep and hope I will wake up and everything will be fine and there will be no bag and they’ll only have to take a small amount and I’ll survive and not have any complications. Oh and remember to breathe!
The anesthetist explains she is going to give me something nice to start with to help relax me. I felt all floaty and gooey and happy and then I feel this coldness creep up my arms, like you’re putting your fingers, then palm, wrist, forearm into a bucket of water and ice. I then feel and see my eyelids start to droop as I blink and I am gone”¦
”¦what seems like seconds later but was actually over three hours I am then waking up in recovery and I feel sick!!
A recovery nurse comes over and asks how I feel and through the oxygen mask I mutter about feeling sick and I’m immediately given some anti-sickness drugs into my arm that provides instant relief. My next question to her”¦ “Have I got a bag?” and I instinctively reach down to feel if there is one there. The nurse grabs my arm quickly afraid I’d do some damage and informs me I don’t have one and everything went well.
I’m not sure how long I was in recovery for as I was in and out of sleep, but I remember the porters coming for me and taking me back to the ward and onto the HOB - high observation bay - which is where all post-op patients go to be observed. I’m told about the strange cylinder I’m holding in my hand. This is my morphine pump and whenever I feel pain and need some relief I’m to push it and I won’t overdose as it’s on a timer. So I give it a go and I don’t remember if I was feeling pain or not (the spinal block was really good) all I can remember is feeling a tightness and pinching around my abdomen on my right hand side.
I drift in and out of consciousness all afternoon, I had a quick visitor from a nurse friend who wanted to come check on me and, before I know it, the family have turned up too as it’s now evening visiting time. I remember my mum stroking my hand, my uncle and aunty standing at the edge of the bed (my uncle hates anything to do with hospitals so I am impressed he is there) and that’s pretty much it as I would fall asleep and wake back up again, pretty much in time with when I was pushing the morphine button. Who knows what they chatted to me about and what I said!
Visiting time ends and I seem to rouse a little bit more with the weirdest realisation that I hadn’t been to the toilet for a wee in hours and then remembered I was catheterised and a nurse is emptying my bag at the bottom of the bed.
The first night in hospital is a strange one, I fall in and out of sleep throughout the night as I’m starting to feel really uncomfortable. The pinching feeling coming from my right side is growing and whenever I move it hurts. I’m not used to sleeping on my back so I shuffled around with my arms until I felt they were in a comfortable position. I’m also woken up by a fellow patient (there are six of us in the HOB altogether) who is vomiting badly and he can’t find his call bell so I call mine for him. He sounds really ill and all I want to do is help but I am literally bed ridden and have no use of my legs yet!
This is my first ever stay in hospital and the mornings start early! By 6am there is a hive of activity and it starts with observations, heart rate, oxygen levels and blood pressure and not long after 7am breakfast is served and I’m told I can have something to eat!
I’ve been informed by this point that as part of the advanced recovery practice I am to start eating and moving as soon as possible, definitely within 24 hours as research proves you recover quicker if you get back into eating and moving as quick as possible. With bowel surgery, your bowel actually becomes dormant, it goes to sleep, because it has been touched, cut apart and sewn back together (this is literally what happened) and I’m not allowed to leave until my bowel wakes back up and is passing gas or stools and to do that I need to eat and walk about.
So I eat some cereals and toast quite happily, not an awful lot as they tell me to take it easy and I didn't have a massive appetite.
Next comes bathing”¦ the whole concept of a bed-bath is beyond me but that’s pretty much what happened. The healthcare assistants had to wash my legs for me as I still hadn’t stood yet and they didn't want me getting up just yet. They washed my back and then left me to wash my torso and personal areas! I’m not prudish in the slightest but it was nice to just be able to do something myself as I had handed my body over to drugs, science and other human beings for the last 24 hours and loved that I could do something myself.
Towards lunchtime the nurses asked if I would like to sit in the chair for a while, eat my lunch there and when I was ready get back into bed, which sounded like a lovely idea. It also sounded really simple but of course it wasn’t”¦I wasn’t allowed to bear any weight on my legs, I had an IV in one hand, my morphine pump and the catheter with bag to contend with. For the assistants this was a normal thing for them to be doing but not so much for me.
We managed it though and I got into the chair, nice and comfy, had my lunch, watched some tv and then my dad and brother turned up to see me. I’m still using the morphine pump at this point and was still very tired and keep drifting in and out of sleep. They think it’s funny so I don’t feel too bad. I’m put back into bed and stay there for the rest of the day, eating, sleeping and sleeping some more. This was post-op day 1!
Post-op day 2 had a similar theme apart from they want me to walk a small amount today and it’s just bizarre being a 28-year-old guy having to hold on to somebody to help me walk literally 100 yards and back to my bed again and that was it...that was my walk. I used to run 8k on my own but could not walk 100 yards without assistance. It’s crazy what can happen to your body - but also adds into perspective how we should look after what we have been given. I eat, bathe, sleep, speak to visitors and before you know it, it’s bedtime again.
Sunday, post-op day 3 and it’s time for the catheter to come out and move into a different bay on the ward! The removal of the catheter is quick and slightly woozy but not painful at all and it’s nice to be able to just have some more control over my body. I’m now walking without assistance to the toilet. I’m eating three meals a day by this point and along with the crisps, sweets, chocolates people are bringing me but still not showing any signs of my bowel waking up. No gas, no bowel movements, nothing, so it’s still a waiting game”¦ I am weighed today though and in 3 days I have lost 7lbs in weight. A nurse tells me your body uses an extra 500 calories a day after surgery to heal properly so if it’s not getting it what it needs then weight loss occurs!
By Monday (post-op day 4) I am starting feel a bit fed up”¦I don’t feel like I have anything new to tell my visitors, unless they haven’t been to see me yet, so we are getting bored of one another - nothing wrong with being honest! By today I am trying to walk as much as possible to get my bowel moving as I just want to go home and also have huge discomfort in my shoulder blades and back. The nurses explain this can be trapped air left over from the surgery. As I had keyhole surgery they pump you full of air to get around with their instruments and they cannot get it all out so it sits in your body trying to get expelled.. so another reason for all the walking. The walking is exhausting though and my parents both tell me to calm down, take my time, listen to my body and be patient”¦as I am walking them out of the hospital!
I wake Monday night, early Tuesday morning, thinking the time has arrived and that my bowel had woken up, so off I hobble to the toilet and wait”¦.. suddenly though I was throwing up a black, foul smelling mess onto the toilet floor which was bizarre as I didn't feel sick at all. Embarrassingly I have to call someone to come clear up after me and head back to bed.
The nurse comes to visit me and ask how I am feeling and I am very nauseous so I’m given an anti-sickness drug in my IV which I feel going to work straight. My throat becomes really dry and my stomach and feelings of sickness just disappear so I fall back to sleep.
When I wake Tuesday morning, post-op day 5, I am still not feeling great. I’m not hungry, pass on breakfast altogether and I am hot, boiling hot. I have no energy to get up and walk about and just lay in my bed wondering what is going on. From my observations I’m running a high temperature and they think I may have a post-op infection so I have blood tests. Team of doctors also arrive and ask whether my bowel has woken up yet and he asks if I have vomited at all. It’s like he was psychic as I’d not been asked this for the past 4 days but today I was. I told him I was very early this morning and he decided there in that moment I needed to have a NG tube fitted. I had read about NG tubes in blogs before my surgery. It stands for naso-gastric, which means a tube down your nose into your stomach. The aim is to empty my stomach and bowel and let it rest in an empty state”¦which means what I vomited the night before was the contents of my bowel! Because it wasn’t moving through the bowel, my body was now rejecting it another way and that was through my mouth.
I was really worried about having this fitted, I had no idea what it would be like and the thought of having a tube inserted into your nose and then passed down your throat didn’t sound like a nice experience”¦and it wasn’t.
My aunt and uncle were visiting at the time the nurses arrived to fit the tube and were asked to go wait in the day room whilst they inserted it. They measured the tube from my nose, past my ear and down to my abdomen and noted around the number 50 on the tube. I was given a cup of water with a straw and told to sip the water as they passed it through my nose and into my throat so it would go down there and not into my windpipe. The first attempt didn't work and I started to choke so they pulled it back out and allowed me to catch my breath. Anxiety was now at an all time high. I can still remember the feeling of the tube passing the back of my throat! Second time round it works and it goes down my esophagus and into my stomach. The other end is attached to a bag and then a vacuum created by a syringe pulling through liquid so that it completely empties my stomach and bowel - so the nasty brown substance I left on the bathroom floor is now to pass up the tube into a bag on the side of the bed.
My aunt and uncle come back and I’m not much company. The tube is really irritating on the back of my throat and I’m swallowing constantly to try get it feeling more comfortable and I’m really tired from the whole ordeal! There isn’t much time left of visiting anyway so off they go and I get into bed to try have a snooze. I’m now nil-by-mouth and not allowed any food at all to rest my bowel. Between the snoozing, constant swallowing and sipping of water to try to relieve the irritating itch-like feeling at the back of my throat it’s almost time for evening visits and my folks will be coming again. I’ve pre-warned them what to expect - mum isn’t the best in hospitals and I know she won’t like seeing me like this. I’m laid in bed about half an hour before they are due to arrive and I all of a sudden sit up in my bed and vomit the black, bowel substance all over myself, the bed, my clothes and the floor. Which shouldn't be happening as it should all be going into the tube and into the bag!
I’m cleaned up, put into the chair and a gown, bed changed all in super speedy time ready for my parents to arrive. Seeing them arrive brings tears to my eyes and I remember so well wanting them to just pick me up and take me home, back to my old bedroom at their house and be looked after by them. I immediately know I mustn’t look great as mum looks incredibly sad and even my dad is somber - he’d normally be making a joke about tubes in noses or asking how it was done but he comes and sits next to me and asks how I am.
I don’t remember what we talked about but I do remember them helping me back into bed before they leave for home and there was something so comforting about my parents putting me into bed, it felt natural, right, their thing to do, no-one else. They had done it for the first decade of my life in every situation so why not now in a time of need and comfort?
The comfort doesn’t last very long. Not long after mum and dad leave I vomit again and the nurse visits this time and notices the NG tube isn’t down far enough and that’s why I am vomiting. So it’s pulled out and a new one has to be reinserted, this time they measure 70cm instead of the 50cm like before. This nurse has done this many times and puts me immediately at ease. We do it slightly differently this time and every time I sip the water she pushes it down so it’s not as irritating and we stop halfway for me to rest before the rest goes down, sip by sip. I start to relax slightly now, the feeling of the tube there is still annoying as hell but the liquid seems to be coming through more often now which means the vacuum is working. I’m told if I feel sick again to let them know and they will keep pulling through the liquid with the syringe as that should stop the vomiting happening. I do need this several times through the night and don’t sleep at all but luckily I’m not vomiting all over myself again.
By this point I have also been told I have a post-op infection and they think it’s in my wound which was glued together underneath my belly button. I’m put onto antibiotics that look like they would be given to horses as the pills are so big and early Wednesday morning, post-op day 6, I need IV paracetamol too as my temperature is sky high again.
Then around 6am the moment happens that I’ve been waiting for...I need to use the bathroom, my bowel is waking up. And I needed to go that minute...which was difficult with an IV and an NG tube, but I manage to make it to the bathroom. As I walk back to my bay, my nurse stops me and asks if I have anything to tell her (I swear they are all psychic) and I fill her in! She smiles, tells me it’s good news and to be prepared to visit a lot over the next few hours and that she’ll update the doctors as they start their rounds.
The nurse is right, I visit a lot and it’s a whole mixture of colour, consistency and acidity - yes it’s like I’ve had a very hot curry! Thank God I’ve brought my handy wipes with me as the NHS toilet paper is actually a distant relative of sandpaper!
They thankfully come and remove my NG tube and even though it’s only been in for 24 hours, it was the most uncomfortable 24 hours I think I have ever had and I am so relieved when it is out. I am keeping my fingers crossed that this now means I get to go home when the consultant turn up for rounds later on”¦but it’s a no! Even though my bowel is wide awake now, the infection needs monitoring so they want to keep me in for another 24 hours to see what happens!
I also get my appetite back and the lovely catering staff rustle me up four slices of toast and a cup of tea which are both just heavenly. The rest of day 6 is spent eating, sleeping pretty much all afternoon (as I didn’t sleep the night before) and watching movies!
Day 7 - a whole week since I arrived and I am finally told I get to go home as my wound underneath my belly button where the infection is has burst, which means the antibiotics are working, apparently! So I am cleaned up, dressings are applied, a whole host of medication is handed over including the Fragmin injections I need to have every day for another three weeks. These are to thin your blood to decrease your chances of DVT, especially as I’m not as mobile as I would normally be and I get to go home with a follow-up appointment the next day with the district nurse to check on my wound.
I pack up all my belongings, that have grown since I’ve been in as more “stuff” is brought along and finally get to walk out of the sliding doors and inhale deeply the fresh, crisp February air - and I remember it feeling so good! Good that I was having some fresh air (I’d not ventured outside much over the last seven days), good that I was leaving, hoping not to return for at least a few years and good that I was going home to sleep in my own bed and be surrounded by my own home comforts.
Being home was nice but also slightly odd. No call bell anymore, no bed that would move in different positions to make it easier to get in and out of, the feeling of safety being surrounded by health professionals had gone but it was purely adjustment, I was happy to be home.
The next few days were tiring, I slept a lot as I tried to get back into a normal routine. Normally I would be pottering around the house, entertaining, maybe having a walk but just getting in the shower and dressing left me exhausted.
Over my recovery period things became easier again, I could walk longer, started driving again after four weeks, managed to socialise more and be out for longer periods of time without being too tired. My bowel habits were really inconsistent though, which I took as standard practice seeing as what I had been through but I had very similar symptoms to before the surgery, just without the pain in my abdomen. I spoke to the IBD helpline, sent in stool samples to measure my calprotectin levels and was told that I had slight inflammation but it was not high enough to be anything serious.
In total I had five weeks off work before I finally returned and even then my first two weeks I was able to work from home - and needed it. My first day back I was back on the sofa by 2pm as I was tired enough to sleep. I’m so fortunate in that I can manage my own time and I know that some others aren’t as lucky as me. My advice is always listen to your body, if it needs to rest, rest! The more you push yourself when you’re not at your best, you’ll always end up causing more damage.
At my follow up appointment in May I had experienced more inconsistent bowel habits and when examined by the surgeon, Mr G, he ordered me a CT scan as he could feel swelling internally and was unsure it was left over from the surgery or a reoccurrence of my Crohn’s already.
The CT scan didn’t show anything significant so I carried on. Now it was never as bad as what I was experiencing before the surgery, but I was really surprised that I was having symptoms so soon. This surgery was supposed to (apparently) buy me 5-10 years remission and good health and I’d had less than four months.
The flares kept coming and going and I kept in touch with the IBD team and from one set of calprotectin levels they decided to bring my colonoscopy forward. You normally have this as standard a year after the surgery but they wanted to get a look in before then.
This colonoscopy was a nicer experience than the first I had (still not the nicest thing to go through but nicer and I was well drugged up) and the results were in”¦I was ulcerating again meaning I was no longer in remission.
This may sound strange and I quote this from earlier on, but in some ways, even though I was really disappointed, I was also so relieved that my illness had been proved again. IBD is known as the invisible disease for good reason that sometimes it’s only when the eyes can see it, anything is done about it. To anyone else I look like a normal healthy guy, take a look at the inside though, or a little closer to how I lead my life, and that’s when you start to notice the difference IBD can make.
Dr S, who performed the colonoscopy, sat me down and discussed the use of immunosuppressants, particularly Azathioprine, and he gives me some information documents about this and another drug and asks me to go away and think about whether I want to start treatment. I thought it was a silly question - of course I want to start treatment but then when you start to read the side effects it can cause it makes you pause and wonder if it is the right thing to do. You’re making the choice to stop your body doing its job, its prime function to keep you alive and fight off infection. Azathioprine tones this down and lowers it to a level that makes you more susceptible to infections, colds, viruses and with that comes risks.
I decided to take it though and started the treatment and didn’t really experience any side effects - apart from some nausea if I didn’t take my tablets with food (I was taking one at every meal time) - and once I spoke to the IBD team about this they recommended I had all three just before bed, which I started to do and it solved the problem!
Unfortunately the Aza wasn’t doing the trick though, in 2015 I was admitted to hospital twice and experienced two really bad flares that resulted in the need for steroids to take control and give me some remission. At my three-monthly follow-up with Dr S in October we reviewed my calprotectin levels from my first flare in June and they were at 600, which is much higher than they should be on immunosuppressants. This has now led to me using a biological treatment - Humira. I was given the choice of Infliximab too but this needs to be given via an IV every 4 weeks and it takes pretty much up all of a day as you need to be closely monitored. So I decided on the Humira as it’s administered by injection pen and you can do this at home. Yes that’s right I now inject myself once a fortnight!
I’ve written a Humira diary that you can find on IBDrelief that takes you through my journey with Humira so far, so go have a read if you want to know more about that and what it’s like. Remember it’s just my journey and everyone’s is different, but I know reading about the injection itself was really valuable for me, so I hope some of you find some use from it.
As for the surgery, it gave me what I needed there and then and the remission I got was small, but if I’d not had the surgery then who knows what state I would be in right now. I am well prepared also for the fact I will need surgery in the future. No one has told me that yet for certain but statistically, if you’ve had surgery once for IBD, you’re 80% likely to need more in the future. With my Crohn’s being rated as moderate to severe it just ups the chances. In some ways, I’m glad I’ve experienced it already at an early age, so that if/when the time comes for more surgery I’ll know what to expect and how to deal with myself and the recovery.
There are many types of surgery and its effect is different for each of us, the recovery will be different for any of you who have this surgery, or any other procedure. If you do find yourself going in for surgery, my top tip - take each and every day as it comes. Be really mindful of each day and take it slow, slower than you think you should and don’t push yourself too much. Listen to your body, rest when you need to rest, walk when you feel you have the energy but remember it’s not a race. Our bodies go through enough as it is, the trauma it goes through having surgery is another layer of stress upon it. It is amazing, though (we may not think it at times and curse it until we are blue in the face). It will heal and it will get back to as normal as it can. Then you can go and experience the advantages the surgery has given you and live your life the way your body will allow - hopefully more positively than before the surgery! Enjoy these moments and experiences and make happy memories, smile, laugh and be content.