Do you know where your ulcerative colitis (UC) is located? Did you know the location of your UC can affect what treatment might be best for you? In this article we take a look at the different types of UC and why it’s important you know where your ulcerative colitis is located.
Ulcerative colitis, or UC as it is also known, is a chronic, lifelong condition which is part of a group of conditions known as inflammatory bowel disease (IBD).The underlying cause of UC is unknown.
UC causes inflammation of the gastrointestinal tract (gut). This inflammation can occur in the colon (large intestine), rectum and anus. Small ulcers develop on the bowel’s lining which produce pus and mucus. This can cause abdominal discomfort and diarrhoea (which may contain blood, mucous and/or pus), among other symptoms.
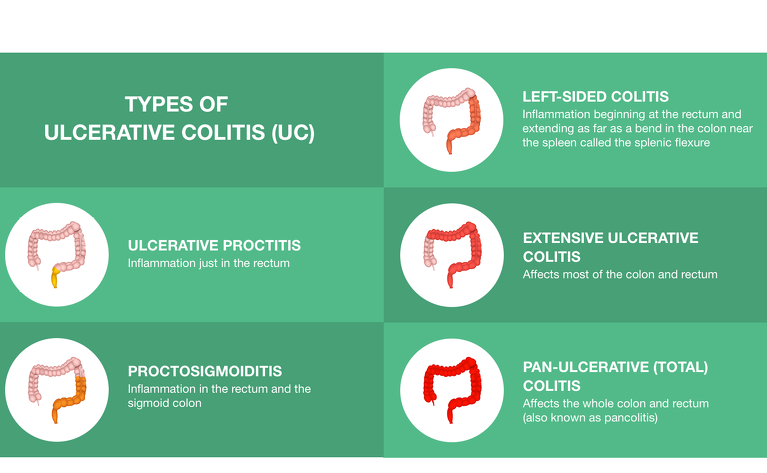
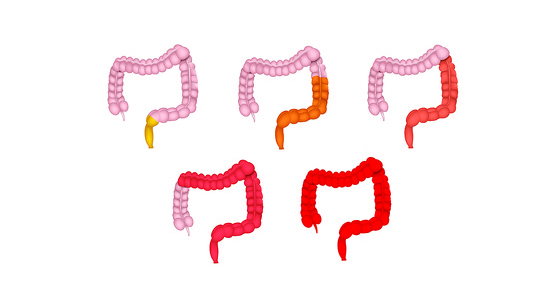
Depending on where you have inflammation will depend on the type of UC you have.
The types are:
Knowing which type of ulcerative colitis is important for a number of reasons
The location of your UC can affect which treatment may work best. If your disease is located at the very bottom end of your colon then rectal treatments, medications you put up your bottom, may be more effective than oral treatments.
There can be subtle differences between the symptoms you experience with the different types of UC. Knowing which type you have and the typical symptoms can help you recognise if a new symptoms might indicate a change in your disease.
Ulcerative colitis is a relapsing and remitting disease. This means you will experience some times of flares (when your disease is active) and some times of remission (when you are well). Over time the location of your colitis could change (either spread into more of the colon or cover less). Understanding more about the type of UC you have can help you to interpret the information from your IBD team so you know if your disease is changing over time.
There isn’t one test that can be done to tell what type of UC you have so your doctor will carry out various tests. This will likely be done at diagnosis, but you will also have regular tests to monitor your disease progression and treatment. These tests can include:
The results of these will be combined with the symptoms you are experiencing to determine the type of UC you have.
If your IBD team doesn’t inform you where your ulcerative colitis is located, or you want them to explain more about the type you have, then you can speak to your doctor or nurse and ask them for more information.
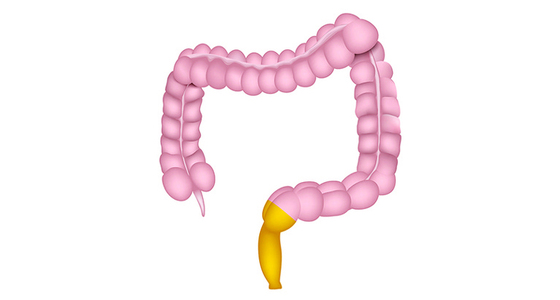
In ulcerative proctitis the inflammation (which can cause sores and ulcers) is in the rectum, the lowest part of the large intestine1.
Typical symptoms include:
Treatment
As ulcerative proctitis occurs in the rectum, some of the best treatments for this type of ulcerative colitis are rectal preparations (medicines you put up your bottom). This is because by inserting the medicine into your rectum it is targeting the inflammation directly where it is occurring. This is known as topical treatment. When you take medicine in a pill form it has to travel through the whole of your digestive system before getting to the rectum and can be absorbed in other areas of your digestive system, as well as the target area.
Rectal preparations you may be prescribed, either when you are first diagnosed or to treat flares, include:
Research has shown that rectal preparations are the best first-line treatment for proctitis, with 5-ASA topical treatments having similar or improved efficacy to the same type of steroid treatment3.
If rectal preparations don’t work, or aren’t tolerated, then oral forms of 5-ASAs and/or steroids may be tried as the next line of treatment.
After this treatments may include:
In proctosigmoiditis the inflammation is in the rectum and the sigmoid colon (the S-shaped lower segment of colon located right above the rectum).
Typical symptoms include:
Treatment
As with ulcerative proctitis, rectal preparations (medicines you put up your bottom) are often recommended over oral medications in the treatment of proctosigmoiditis4. This is because these medications can target the inflammation directly where it occurs. Suppositories are tablets placed into the rectum with a finger, while liquid enemas and rectal foams are ‘squirted’ into the end of your bowel via an applicator inserted into your bottom. The liquid enemas and foam can treat inflammation beyond the rectum, into the sigmoid and left-sided areas of the colon.
These rectal preparations include:
If rectal therapies (also known as topical treatment) are not effective for you, or you find it difficult to take them, then you may be given oral versions of these medications.
If your treatment needs to be escalated further then you may be prescribed an immunomodulator, such as azathioprine, or a biologic therapy.

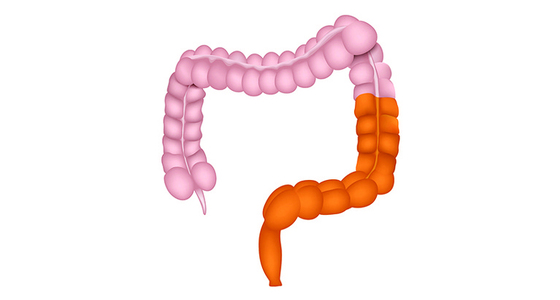
Left-sided colitis is also known as distal colitis and in this type of UC the inflammation begins at the rectum and extends as far as a bend in the colon near the spleen called the splenic flexure.
Typical symptoms include:
Treatment
The first treatments you will likely be given for a flare of distal colitis will be a 5-ASA (such as mesalazine) and/or steroids. You may be given either rectal preparations (medicines you put up your bottom), tablets, or a combination of both. The rectal medicine targets the inflammation in your rectum and the lower part of your colon while the tablets treat inflammation throughout.
As well as treating flare-ups of your disease, 5-ASAs are also used as a maintenance treatment (something you take long-term to keep you in remission).
If these first-line treatments don’t work then you might be given an immunomodulator to take long-term. These include:
Immunomodulators work by dampening down the immune response in your body, in turn reducing the inflammation.
After this, biologics are the next treatment you may try. These include:
Or JAK inhibitors such as:
Extensive colitis and pancolitis are very similar, except extensive colitis affects most of the colon while pancolitis affects the whole colon.
These types of ulcerative colitis can have more complications associated with them.
Typical symptoms include
Treatment
The treatment you receive for extensive colitis or pancolitis will depend on the severity of your inflammation and symptoms.
During a flare-up of your disease the steroid prednisolone is often prescribed orally (tablets) and you may also be given a topical steroid treatment (a rectal preparation that you insert into your bottom) to treat inflammation at the bottom end of the colon at the same time.
5-aminosalicylic acid (5-ASA) tablets or granules are also used to treat a flare and/or maintain remission. Rectal preparations of 5ASAs could also be given at the same time.
If this doesn’t work you may be given an immunomodulator to try to control the inflammation. Immunomodulators for UC include:
Biologics are also regularly used in the treatment of these forms of ulcerative colitis and include:
Or JAK inhibitors such as: