
In this article we take a look at the different locations of Crohn’s disease, the symptoms, specific treatments and why it’s important to know where your disease is located.
Crohn’s disease is a chronic, lifelong condition and is part of a group of conditions known as inflammatory bowel disease (IBD). It causes inflammation of the gastrointestinal tract (gut). This inflammation can be anywhere from the mouth to the anus and most commonly affects the end of the small bowel (the ileum) and the beginning of the colon. It is thought to be an immune-mediated disease (where your immune system attacks a part of your body).
Most patients have Crohn’s disease in the end of the small intestine and the join with the colon. Around a third of people with Crohn’s disease also have it around the anus area.
The symptoms it can cause are varied depending on where in your digestive system your Crohn’s disease is located, but some of the most common symptoms include:
The location of your Crohn’s disease depends on where the inflammation occurs in your gastrointestinal tract. In Crohn’s disease you can have inflammation in multiple places, meaning you could have it in more than one place. It can also change over time as inflammation increases or reduces.
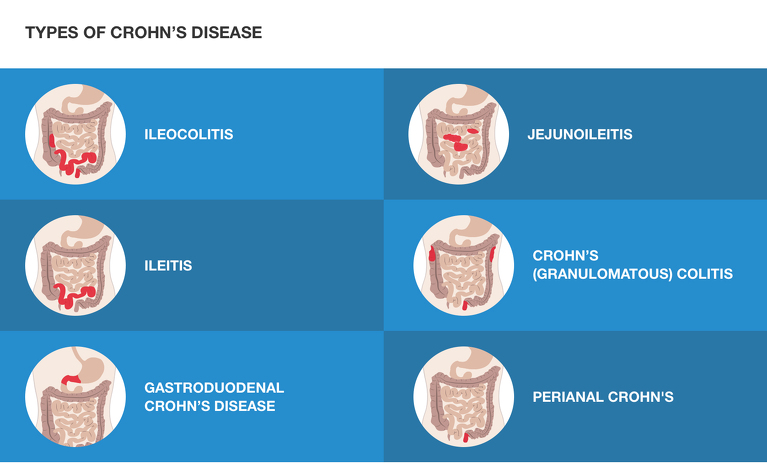
The different locations for Crohn's disease have been given different names to identify them. These are:
You can also get oral Crohn’s disease which affects your mouth.
Knowing which type of Crohn’s disease you have and where the inflammation is located helps you to understand more about your condition and its progression, the symptoms you have and the treatment you may need.
The type of treatment you receive for your Crohn’s disease will depend on where your Crohn’s disease is located. The treatments given for people with Crohn’s disease in the upper part of their gastrointestinal tract can be very different from the treatment for those with it in their rectum. Knowing where your Crohn’s disease is will help you to understand more about why you are given certain treatments.
Knowing the location of your Crohn’s disease can help you to understand what symptoms you might expect and to spot any new symptoms which might indicate that inflammation caused by the disease has spread to a new location.
Crohn’s disease is a relapsing and remitting disease. This means you will go through periods of remission (when you are well) and periods when you are flaring (when you are not well). Understanding more about where your Crohn’s disease is located can help you interpret information from your healthcare professionals so you will know if your disease is responding to treatment.

The location and severity of your Crohn’s disease will be determined through various tests, procedures or scans that your doctor will carry out or refer you for. These may include:
Once your doctor has determined the location(s) of your Crohn’s disease they will use this information to decide on the best treatment for you. Your doctor may not automatically tell you where your disease is located. If they don’t then you can ask them to give you this information and explain it to you if necessary.
Below is an overview of the different locations for Crohn’s disease with more information about the symptoms and treatment.
This is the most common location for Crohn’s disease and affects the end of the small intestine (the ileum) and the large intestine (the colon).
Typical symptoms include:
If you are having a flare-up of your ileocolitis then it’s likely you will be given a 6-8 week course of steroid tablets to get the inflammation under control. Steroids are not a medication that is taken long-term to keep you in remission and they have some serious side effects, which is why you will only be given a short course.
The steroids you may be given include:
*Budesonide has been shown to be an effective treatment for people with Crohn’s ileocolitis with typically less side effects than prednisolone1.
You may also be given azathioprine as a first-line treatment for your ileocolitis. This is an immunosuppressant that works to dampen down the immune system and reduce inflammation. Other immunomodulators similar to azathioprine include 6-mercaptopurine, methotrexate and cyclosporine. These medications can be taken long-term and are known as maintenance treatments, a medicine that works to keep your disease under control and in remission.
Aminosalicylates (known as 5-ASAs), a type of anti-inflammatory, are sometimes used as a first-line treatment in Crohn’s disease, however this is becoming less common as evidence shows they are not as effective in Crohn’s disease as they are in ulcerative colitis2, although they have been shown to have some effect in mild Crohn’s disease or to help after small bowel resection surgery.
If azathioprine doesn’t work then you may be given biologic. There are several different biologics available and many more coming on the market. Biologics available for ileocolitis include:
For Crohn’s ileocolitis that doesn’t respond to treatment surgery to remove the inflamed parts may be an option.
This affects only the small intestine (the ileum).
Typical symptoms include:
The treatments for ileitis are very similar to those of ileocolitis (listed above)
This affects the stomach and the beginning of the small intestine (the duodenum). Less than 6% of people with Crohn’s disease have it in this location3, with some studies suggesting as few as 0.5-4%4. Although rare, you can get Crohn’s disease in your oesophagus (throat). The majority of people with upper GI Crohn’s disease also have Crohn’s disease lower down in their digestive system5.
Typical symptoms include:
The treatments for gastroduodenal Crohn’s disease are also very similar to those of ileocolitis (listed above). However, 5-ASAs are not considered an effective therapy for this type of Crohn’s disease6.
You may also be prescribed a proton pump inhibitor (PPI) to help manage some of the symptoms of your gastroduodenal Crohn’s disease. PPIs do not reduce the inflammatory response7 so should be used in combination with another medication to treat the inflammation from your Crohn’s disease.
This affects the upper half of the small intestine (the jejunum).
Typical symptoms include
As steroids are not a long-term treatment you will likely be given an immunomodulator (such as azathioprine) or a biologic (such as infliximab or adalimumab) to take long-term to keep you well.
This affects the colon (large intestine) only. The name - Crohn’s colitis - can be confusing leading some people to think they have both Crohn’s disease and ulcerative colitis. However, the word colitis simply means colon inflammation.
Typical symptoms include:
Steroids may be used to treat a flare up of Crohn’s colitis. You may be given oral or rectal preparations or a combination of both. Rectal preparations are particularly helpful to treat inflammation in the lower part of the colon, rectum and anus. You insert them into your bottom and they treat the inflammation directly where it is occurring, while tablets need to travel through all of your digestive system.
Steroids can only be taken for a short period of time and ideally not for more than two courses a year. This means you will likely need a maintenance treatment (a medicine to keep you well). The first line maintenance treatment for Crohn’s colitis is an immunomodulator such as azathioprine. This is a tablet you take daily that suppresses the immune system.
The second line treatment for this Crohn’s disease location are biologic medications, medicines that alter your immune response. The biologics available for Crohn’s colitis include:
Perianal Crohn’s disease causes inflammation around the anus and is another common location. It can occur alongside Crohn’s disease in other locations and it can also occur on its own.
Typical symptoms of perianal Crohn's include:
Other symptoms may occur over time. Some of these advanced symptoms include:
As perianal Crohn’s disease affects the very bottom end of the gastrointestinal tract you may be given rectal steroids. These are steroid medications that you insert into your bottom. They come in suppositories (a bullet shaped tablet) and foam and liquid enemas which you squirt into your bowel using an applicator that you insert into your bottom. Steroids are used to treat flare-ups of Crohn’s disease, but are not a long-term treatment.
To help keep you well long-term you may be given an immunomodulator (such as azathioprine or mercaptopurine) or a biologic therapy (like infliximab or adalimumab).
Antibiotics may also be used if you have an abscess to help stop it getting infected. Surgery is also an option to treat complications such as fistulas and strictures.