Travelling to some destinations means you may need to get vaccinations before your trip. This article takes a look at getting travel vaccinations when you have inflammatory bowel diseases like Crohn’s disease and ulcerative colitis.
The vaccines that you will need for your trip depends on many things. This will include where you are travelling to and when. You are more at risk of catching certain diseases in some countries, and this can increase at different times of the year. It will also depend on what you are planning to do on your trip. If you are staying in a 5* hotel and not planning to leave you may need a different vaccination schedule to someone who is spending their time trekking in the jungle. The vaccinations you have previously received and the medication you are taking will also play a part.
Many countries have a routine vaccination programme (some compulsory, others voluntary) so you may find that you have already been given the suggested vaccinations or only need to have a booster dose.
In short, the vaccinations that you will need will be different from someone else.
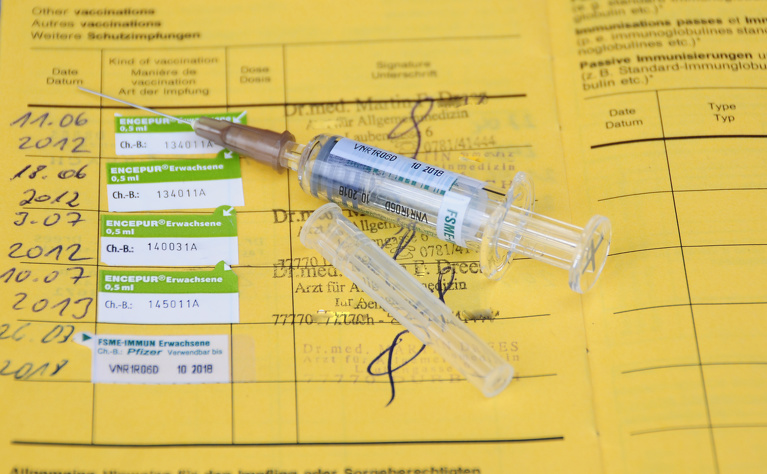
The best way to find out what vaccinations are needed is to speak to a specialist travel clinic at least eight weeks before your trip. They will be able to advise you on any travel-related infectious diseases you may encounter and what precautions you should take (such as having vaccinations). The majority of vaccinations are given as injections.
The NHS Fit for Travel website has a country-by-country guide vaccinations and infectious disease risks. The World Health Organization website also has information about recommended vaccinations and disease risks.
You can also search for vaccination advice and healthcare arrangements by country on the IBD Passport website.
You can have vaccinations if you have inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis, however if you are immunocompromised (your immune system is impaired or weakened) you may not be able to have live vaccinations. Certain medications taken for Crohn’s disease and ulcerative colitis can cause you to become immunocompromised. If you are unsure you should speak to your IBD specialist who will be able to advise you about whether you are considered immunocompromised and to what degree.
Live vaccinations also can’t be given to people who are due to start immunosuppressant medications within the next three weeks.
Many of the medications that are used to treat Crohn’s disease and ulcerative colitis work by suppressing the immune system. These medications are known as immunosuppressants (or immunomodulators). These medications include:
Vaccines come in a few different types. These are:
If a vaccine is live it means it contains a weakened (attenuated) form of the virus that infects you. It works by introducing a weakened version of the virus into your body so that you can develop a long-lasting immune response, without you developing symptoms of the disease you are trying to prevent. This can often be achieved with just one or two doses of the live vaccine. Common live vaccines include:
Inactivated vaccines use a version of the virus that has been killed. These vaccines also try to build immunity against the virus, however it’s not usually as long-lasting as a live vaccine. You may need several doses and/or boosters to have ongoing immunity.
Common inactivated vaccines include:
Subunit, recombinant, polysaccharide and conjugate vaccines use certain pieces of the germ from the virus. They give a strong immune response to these targeted pieces of the germ. Like inactivated vaccines you may need boosters to retain ongoing immunity.
Common Subunit, recombinant, polysaccharide and conjugate include:
Toxoid vaccines use a toxin made by the virus that causes a disease. Immunity is created from the parts of the germ that cause a disease instead of the germ itself. Again, you may need boosters to retain ongoing immunity.
Common toxoid vaccines include:

If you have a live vaccination while your immune system is suppressed from taking immunosuppressant medications then you run the risk of becoming very ill.
If you are yet to start taking any immunosuppressant medication then you may wish to consider getting vaccinated against some diseases before starting, especially if you have a desire to travel in the future. Your IBD team can advise on how long you should wait before starting the new medication after having a live vaccine, but general advice is at least three weeks1.
For those who are already taking immunosuppressant medicines then you should speak to your IBD doctor about whether it is advisable to stop your medication in order for you to have any live vaccines. Guidelines suggest waiting 3-6 months after stopping the medication before having the vaccinations and then waiting another three weeks before restarting1.
Many vaccinations are only recommendations and you do not have to prove you have had them to enter a country. However, if you decide to do this you should weigh up the risks to your health if you were to catch the disease. For some destinations polio and/or yellow fever vaccinations are mandatory and you must show a certificate to prove you have been vaccinated. An inactivated polio vaccination is available, meaning you can have this if you are immunocompromised. But, yellow fever is only available as a live vaccination. If you are travelling to a country that requires you to have a yellow fever vaccine, and there is no way you can stop your medication long enough to have the vaccination, then you will need to get a letter of exemption from a healthcare professional. You should speak to your GP or travel centre about this. However, this is still no guarantee that you will be given entry into the country. In this case you may wish to consider travelling to another destination. Some countries also request that you prove you have been vaccinated against yellow fever when entering from another country which has yellow fever present.
Being immunocompromised also means that you are more susceptible to getting ill from infections generally, including those you may catch while travelling abroad. This means you may wish to take extra precautions, such as regularly washing your hands, ensuring the food and water you are having is safe.
If you are pregnant, think you are pregnant or breastfeeding you should tell your GP or travel clinic before having any vaccinations. It’s unlikely that you will be given any vaccinations, however this is decided on a case-by-case/risk basis.
This varies on the vaccinations you need and the country where you live. In many countries some vaccinations are free as part of a general population vaccination programme, however there will be others that you need to pay for.
More information about travel vaccinations and those which are free for UK residents is available on the NHS website.
You may be refused entry in to some countries if you cannot prove you have received the vaccinations or show a certificate of exemption. There are some countries that will not accept an exemption certificate, so you should check requirements before travelling. Some countries require proof of vaccination (for example, for polio or yellow fever vaccination), which must be documented on an International Certificate of Vaccination or Prophylaxis (ICVP) before you enter or when you leave a country.
Malaria is present in over 100 countries around the world, including:
Malaria is transmitted by mosquitos when they bite you. There is no vaccination to prevent malaria, however you can take anti-malaria tablets. Generally these need to be started before travelling and continued for a period of up to four weeks after returning. There are various different types of anti-malarial medications and you should talk to your doctor or travel centre about which are best for you, the area you are travelling to and your inflammatory bowel disease.
Some types of anti-malarials cause side effects such as tummy upsets and sun sensitivity.
If you are taking methotrexate for your Crohn’s disease or ulcerative colitis you should be aware that the anti-malarials Daraprim and Vibramycin (Doxycycline) can interact with it. You should declare any medications to your doctor or travel clinic before taking anti-malarial tablets.
The best prevention is to take precautions against getting bitten by mosquitos. Cover you arms and legs, use insect repellent and mosquito nets.
References



