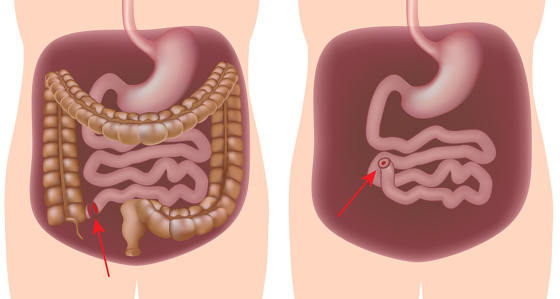
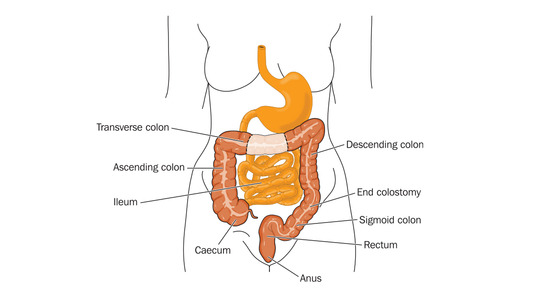
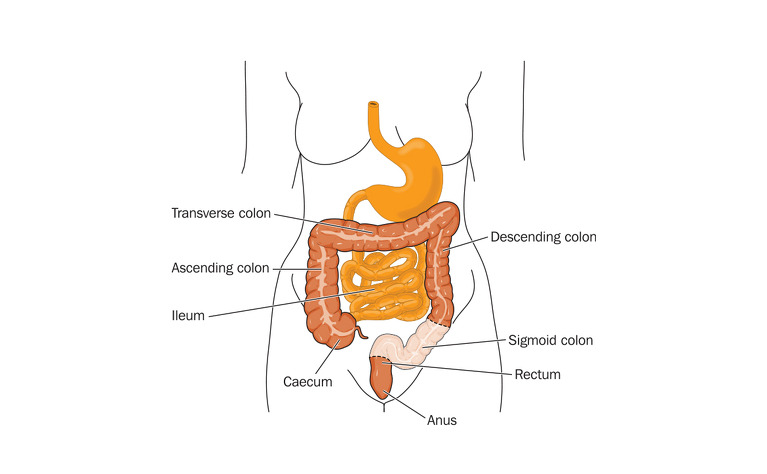
Sigmoidectomy surgery removes all or part of the sigmoid colon - the S-shaped part of the large intestine just before the rectum. Where possible the two healthy ends of the intestinal tract are then rejoined. If this is not possible then a stoma may be formed.
It is also known as a sigmoid colectomy or sigmoid colon resection.
All forms of ulcerative colitis and Crohn's disease affecting the large intestine (colon) - Crohn’s (granulomatous) colitis and ileocolitis.
If your inflammatory bowel disease (IBD) is not responding to other treatments - such as medication - or you have severe inflammation or damage to your sigmoid colon then surgery may be needed.
Shortly before your surgery your blood pressure and breathing will be monitored and you will be prepared for theatre. You may be given medicine through a vein in your arm. Just before the surgery you will be given a general anaesthetic which will put you in a sleep-like state so that you won’t be aware of what’s happening.
Sigmoidectomy surgery can be carried out either through open surgery or laparoscopic (keyhole) surgery. The type of surgery you receive will depend on your circumstances and the surgeon you have. It should be discussed with you prior to your operation.
Open surgery: An incision will be made along your abdomen to provide access to the colon for your surgeon. They will then identify the damaged section of the sigmoid colon and remove it.
Laparoscopic surgery: Several small incisions (or ports) are made in the abdomen. A small camera is inserted through one of the ports to direct the surgeon to the colon. Surgical instruments are inserted through the other incisions and the damaged piece of the sigmoid colon is pulled through one of the ports and operated on externally, before being reinserted. This type of surgery is meant to result in a quicker recovery time for the patient and also less external scarring. In some cases the surgeon will discover during surgery that they need to convert to open surgery due to unforeseen circumstances.
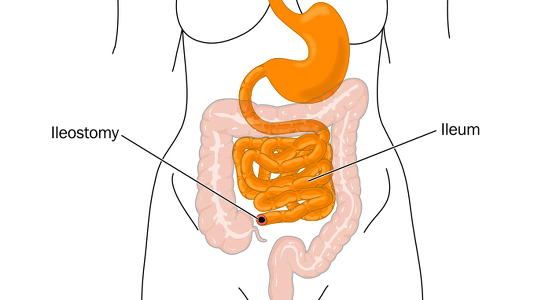
Once the surgeon has removed the damaged parts of the sigmoid colon the intestinal tract must be reconnected. Generally in this type of surgery it is possible to reconnect the healthy ends of the bowel so that your stools can continue to pass through your body in the normal way. However, there are occasions when stoma formation may be needed. If too much of the bowel has needed to be removed, or if the surgeon feels your bowel needs time to heal before it can be reattached, then they may create a stoma. This could be permanent or temporary.
For the first 24 hours following surgery you may find you have an intravenous drip to provide you with fluids and a catheter inserted into your bladder to drain urine. Often an epidural is used to provide pain relief immediately following the operation. This numbs the body from the waist down.
You should be able to eat and drink very soon after the operation and you will be encouraged to move around as much as you are comfortable with.
People recover at different speeds, but generally you will remain in hospital for between 2-5 days if you have had keyhole surgery and 5-7 days for open surgery.
If external stitches or staples have been used to close the wound then these will usually be removed 10-14 days after the operation.
After leaving hospital you will encouraged to continue moving around but to avoid heavy lifting or increased physical activity for about 6 weeks. Many people can start driving again after around 2 weeks.
It will probably take some time for your bowel movements to settle down. It is very different for everyone. Your doctor will be able to discuss with you what you should expect.
With any operation there are risks. These can include: