If you have just been diagnosed with ulcerative colitis you will probably have lots of questions and may feel a bit scared or confused.
This article aims to answer many of the questions you will have if you are newly diagnosed with ulcerative colitis and provide you with links to more articles where you can read in depth about the different subjects covered.
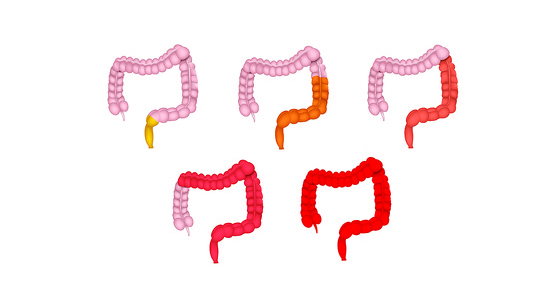
Ulcerative colitis, or UC as it is commonly known, is a chronic, lifelong condition which is part of a group of conditions known as inflammatory bowel disease (IBD). It causes inflammation in all or part of the large intestine (colon, rectum and anus). Small ulcers can develop on the lining of the large intestine which produce pus, mucous and blood.
Colitis means colon (col) inflammation (itis) - hence the term colitis.
Ulcerative colitis is thought to be an immune-mediated disease (where your immune system attacks a part of your body). The other main form of IBD is Crohn's disease.
The symptoms it can cause are varied, but some of the most common include:
Find out more about ulcerative colitis
Most people when they have just been diagnosed with ulcerative colitis are already experiencing symptoms of diarrhoea.
Now that you have been diagnosed your doctors will work with you to get your ulcerative colitis under control so that you have no symptoms and you have a better quality of life. This is known as remission.
With ulcerative colitis you can expect to have times of remission and times of flare (when your symptoms return). We don’t fully know what causes people to have flare ups of their ulcerative colitis. There are patients who report they are more likely to flare when they are stressed or unwell, however others say that they don’t seem to have a pattern.
The treatment you are given will aim to get you into remission and get rid of the inflammation in your large intestine, but it can take time for this to happen. You may find that you need to try a few different medications before you find one that works for you.
During an ulcerative colitis flare you may find it difficult to do day-to-day activities such as work, school or that it may interfere with your relationships. If this is happening on a regular basis, or it is seriously affecting your ability to live your life, then you should speak to your doctor about whether there is another treatment which may work for you or what support is available to you. They may also be able refer you for extra support from psychologists and dieticians.
Right now you may find it difficult to imagine having a normal life again, but it’s important to remember that there are many people with ulcerative colitis who are living their lives - getting married, having children, pursuing education and careers. Talking to people such as your doctor, friends or family about your concerns and fears may help you to accept and understand how you are feeling.

There is no cure for ulcerative colitis and it is something you will have for the rest of your life, so the aim of treatment is to get your symptoms under control and into remission.
All ulcerative colitis patients are different and a treatment that works for one may not work for another, therefore you may need to go through a period of ‘trial and error’ to find a medication that works for you. If the first treatment you try doesn’t work for you then you may feel frustrated and disheartened and that's understandable. There are now many different medication options available and more being licensed for ulcerative colitis all the time so there are now more options available to you than ever.
There is a new test available to people newly diagnosed with Crohn's disease called PredictSURE IBD. This biomarker test can help to predict whether you will have a more 'mild' or 'aggressive' form of the disease. Your doctor can then use these results to help them choose the most appropriate course of treatment for you, hopefully resulting in a reduction of this period of trial and error before they find a medication that works for you.
The first medicine you will likely be given when you are newly diagnosed with ulcerative colitis is steroids (corticosteroids). Steroids normally start working within days of taking them and they tend to reduce the symptoms in the majority of ulcerative colitis patients. However, taking steroids can produce some significant long-term side effects, meaning they can’t be taken for long periods of time or on a regular basis. When starting you on steroids or after taking them for a few weeks it’s likely that your doctor will talk to you about taking another medication at the same time which is slower acting (taking weeks or months to start working), but can be taken long-term. Which medicine you are given will depend on the severity and location of your ulcerative colitis.
Find out more about medications for ulcerative colitis
In some people the inflammation caused by ulcerative colitis can cause irreversible damage to the large intestine. In some cases the only way to treat this is through surgery to remove the damaged parts. The surgery can vary from having the damaged part of the colon removed and the two ends reconnecting (called a resection) to removing the whole colon and having a stoma formed (by bringing the end of the bowel to the surface of the abdomen and using a pouch to collect bowel waste).
There isn’t a specific diet for ulcerative colitis and the role that food plays in UC isn’t fully understood. More and more research into food and ulcerative colitis is being carried out all the time. What we do know is that the food you eat doesn’t cause ulcerative colitis to develop (although it may be one of the many environmental factors that could contribute to its development), however we don’t know for sure how the food we eat affects ulcerative colitis flares and remission.
Many patients do anecdotally say that they avoid certain foods because they feel these foods exacerbate their symptoms, however there are very limited studies to support this and patients are encouraged to make sure they eat a well-balanced diet, including fibre, and do not cut out entire food groups without talking to a specialist dietician.
At times you may be advised by your doctor or dietician to follow a specific diet, such as when preparing for a colonoscopy or after having surgery.
It’s important that you follow the treatment plan set out by your doctor to help treat your ulcerative colitis, however some patients have also found making some adjustments to their lifestyle have been helpful.
Examples of lifestyle changes include:
Before you make any changes you should talk to your gastroenterologist to make sure they aren’t going to interfere with the treatment you are receiving.