
If you’ve just been diagnosed with ulcerative colitis you may be wondering ‘just how serious is UC’? In this article we take a look…
Unfortunately ulcerative colitis, or UC as it’s often referred to, does have the potential to be a serious illness due to some of the complications it can cause.
However, it’s important to remember that most people with ulcerative colitis don’t experience some of the more serious complications that can occur due to receiving effective treatment. To help minimise your risk of complications you should follow the treatment prescribed by your doctor.
Some of the things that can cause serious complications include...
It’s common for people with ulcerative colitis to have vitamin and mineral deficiencies. There are a number of reasons why:
Not getting the right nutrients from your diet can lead to malnutrition which can be a serious condition. Malnutrition generally causes weight loss, tiredness, weakness and causes you to get ill often. Some people with malnutrition find that they don’t lose weight, which can often lead to the problem being missed.
Read more about vitamin and mineral deficiencies
Having PSC and ulcerative colitis is common. It is a liver condition where the liver’s bile ducts decrease in size over time due to inflammation and scarring (known as fibrosis). Often people with primary sclerosing cholangitis don’t experience any symptoms in the early stages of the condition. The most common early symptoms are tiredness and discomfort in the upper right abdomen. These symptoms can be difficult to distinguish from your ulcerative colitis symptoms. For this reason, some IBD doctors do blood tests with UC patients to check for the disease. As PSC progresses symptoms include:
PSC can lead to liver failure, meaning a liver transplant is needed. There isn’t currently a cure or specific treatment for primary sclerosing cholangitis. There are some treatments available to treat some of the symptoms.
The exact reasons why PSC is more common in people with ulcerative colitis isn’t fully known. It’s thought that it may be because whatever causes ulcerative colitis is the same or similar to the cause of PSC, or that having inflammation in your colon allows toxins or infection to be absorbed into the body, leading to bile duct inflammation2.
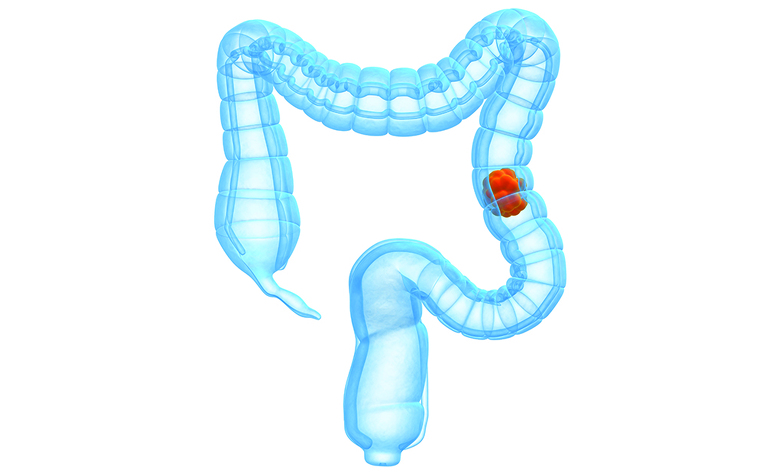
Having ulcerative colitis can increase your risk of developing bowel cancer, however how much your risk is increased by depends upon:
The general population has a risk of around 4.5% of developing bowel cancer in their lifetime. One large meta study showed that the risk for people with UC is around 18% after 30 years of UC symptoms3.
Read more about ulcerative colitis and bowel cancer
This very serious complication is rare, but it’s important you are aware of its symptoms as it can be a life-threatening medical emergency.
Toxic megacolon is where the colon becomes swollen due to trapped gas and/or faeces caused by excess inflammation preventing it from passing through. The swelling can cause the colon to rupture or may lead to the blood infection septicaemia.
Symptoms of toxic megacolon include:
Treatment can include intravenous fluids, antibiotics and steroids, as well as a tube inserted into the anus to relieve built up gas. In serious cases the colon may need to be removed, resulting in a colectomy with a stoma.
Around 20% of people with ulcerative colitis will require surgery at some point4. The most common surgeries for UC are:
Having any surgery carries a risk of complications. These can include:
If you are having surgery for ulcerative colitis your surgeon will talk you through the associated risks.

Reading through some of the complications you can get from ulcerative colitis may seem scary, however there are some things that you can do to help minimise your risk. These include:
One of the biggest risk factors for developing complications in ulcerative colitis is uncontrolled inflammation, either because the medication being taken isn’t working or because the patient isn’t taking the medication as prescribed.
To help target treatments better there is now a blood test available called PredictSURE IBD which can help predict the likely severity of your ulcerative colitis. This can help your doctor to target your treatments early on. It can also give patients who are predicted to have milder disease more confidence in receiving less frequent monitoring from their IBD team.
Ulcerative colitis is not considered to be a life-threatening condition, but some of the complications listed in this article can be. Developing infections such as sepsis, bowel cancer or toxic megacolon could cause you to have an increased risk of death slightly over the general population. By taking your medication as prescribed and seeking early treatment for new symptoms you can help to reduce these risks.
Harvard Health Letter: Are your medications causing nutrient deficiency? https://www.health.harvard.edu/staying-healthy/are-your-medications-causing-nutrient-deficiency
British Liver Trust https://britishlivertrust.org.uk/information-and-support/living-with-a-liver-condition/liver-conditions/primary-sclerosing-cholangitis/
Surgical Principles in the Treatment of Ulcerative Colitis, Florian Kühn and Ernst Kla. Viszeralmedizin. 2015 Aug; 31(4): 246–250 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4608637/