Magnetic resonance imaging (MRI) is a common test used in inflammatory bowel disease (IBD), particularly Crohn’s disease, to take a look at the small bowel (and sometimes colon). It is especially good at looking at the ‘extra-luminal’ complications of Crohn’s disease (complications that penetrate through the intestinal wall). This compliments a colonoscopy well, as it can only look at the surface of the bowel.
As with all areas in healthcare, MRIs are evolving as new technology becomes available. In this article we take a look at how the images from MRIs are currently reviewed by healthcare professionals (HCPs) and some new technology that is becoming available to help improve things for both HCPs and patients.
In IBD MRIs are broadly used to tell a healthcare professional (HCP) three things:
Where the disease is located - is it in the small bowel, colon, both or elsewhere?
What is the disease doing - is it causing strictures, fistulas?
How active is the disease? Would the patient benefit from medications, is it better to perform surgery or would doing nothing be OK?
MRIs are very good at helping with the first two of these, however they struggle with the third. For this endoscopy is a better option, but the small bowel is inaccessible using this method. It also isn’t an ideal option in young patients who would receive a general anaesthetic to undergo it. To help solve these issues advances in MRI are important as the medical world moves towards more precision medicine in the management of Crohn’s disease.
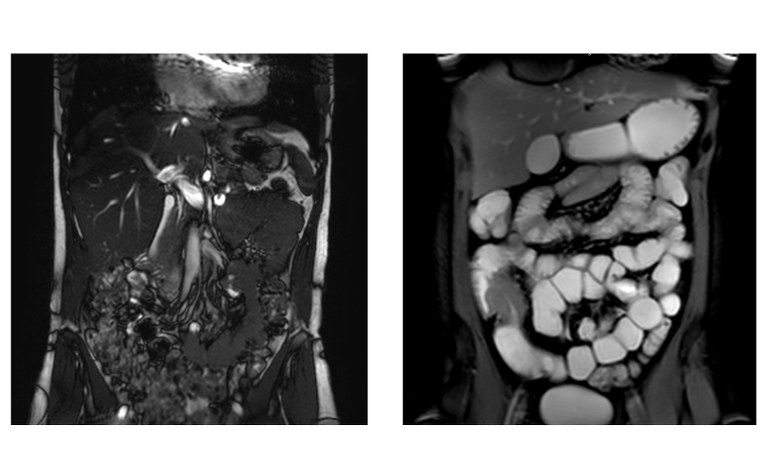
As a patient having an MRI you will be asked to lie in a tube-shaped machine and follow the instructions given to you by the radiographer. This may involve holding your breath or holding still at certain times. While you are doing this the radiographer, a healthcare professional trained in imaging, will be taking hundreds of cross-sectional images (known as slices) of areas of your body (in IBD this is usually your small bowel). These will be done along several different axes of your body, which is why an MRI scan can take some time.
Once all the images have been captured they are sent to a radiologist, a doctor trained in analysing the images. The pictures are layered together to form 3D images of the parts of your body that are being looked at. Using their years of training and experience, the radiologist studies your scans, looking for areas of inflammation or other changes to the bowel and other body parts pictured (points 1 and 2 in the ‘Why are MRIs used in IBD’ section above).
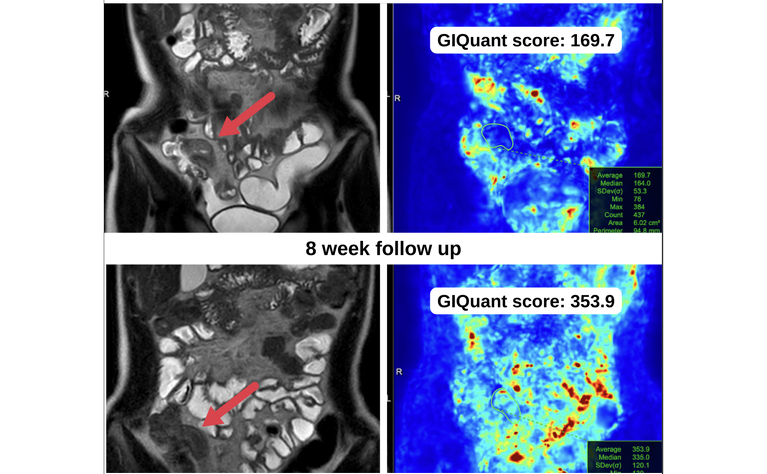
They then write a report based on what they have seen from your scans. This report includes details of their interpretation of your scan and is sent to the doctor or healthcare professional (HCP) who requested the scan. The report details information about any abnormalities in written form, but there isn’t currently a standardised way of giving HCPs and patients a measurable score to track any changes to the bowel over time (such as an inflammation or disease activity score). This can mean changes may not be identified until they become visible to the radiologist's trained eye. As a result it is not necessarily quickly known if a patient is responding to a new medication or has stopped responding to a current medicine.
Emerging technology in the MRI field is currently trying to address some of these challenges and limitations of the current system and to move us closer to precision medicine.
One of the companies doing this is Motilent. Motilent has developed technology, called GIQuant, which can give a score for a patient’s Crohn’s disease activity based on their MRI scan images. This score can help to track how a patient is responding to treatment over time, potentially reducing the amount of time a patient may spend on an ineffective therapy. The technology can even be applied to some previous MRI scans to provide an historic overview of disease activity.
GIQuant uses computer vision, a way of training machines to do the job of the human eye and get a high level of understanding from digital images or video, to generate the scores. This technology also means it may decrease the time it takes to carry out MRI scans and reduce the need to have injections of spasmolytic medicines such as Buscopan and gadolinium during the scan.
In summary, this is sophisticated technology made simple and now available across a range of NHS centres that increases the capacity of existing equipment and is one of a number of advancements we are likely to see making their way into Crohn’s disease care in the near future.
GIQuant is already in use in some hospitals in the UK, working to support healthcare professionals to improve services, efficiency and speed of diagnosis, monitoring and treatment.
And, as the pressure on healthcare continues to mount, we may start to see wider usage of machine learning and artificial intelligence solutions to help improve efficiency so HCPs can attend to more patients.
Crohn’s disease is complex and management of the condition still has a long way to go. Emerging technologies like GIQuant are helping with advancements and part of a wider push to continually strive to improve outcomes for patients.