It’s not uncommon for people to still experience gastrointestinal issues when their Crohn’s disease or ulcerative colitis is shown to be in clinical remission by their doctor.
Clinical remission means tests show you currently have no active inflammatory bowel disease. This is often measured through faecal calprotectin, CRP blood tests and/or endoscopy tests.
So, if you are told you are in clinical remission but are still suffering from symptoms such as diarrhoea, bloating, nausea and sickness why might this be?
There are a number of different reasons why this could be - and it may not even be related to your IBD.
Some of the things which could be causing your symptoms are:
Scroll down for more information on each of these...

It is possible to have both IBD and IBS, though many people often don’t realise they have both as they put their gastrointestinal symptoms down to their IBD.
IBS is a common (it is thought to affect at least 10-20% of adults in the US) functional disorder of the colon which results in chronic, painful spasms which can move from one location to another. Unlike IBD, IBS does not cause inflammation, however it can result in some similar symptoms to IBD - such as cramping, bloating, diarrhoea and constipation - which is why people can sometimes be wrongly diagnosed with IBS when they actually have IBD.
Because IBS does not lead to disease or cause any inflammation or ulcers it doesn’t do any damage to the bowel, cause intestinal bleeding or harmful complications which can be seen in IBD. When examined the bowel of someone with IBS looks normal - it just isn’t functioning in the correct way.
Some people with IBS find that certain things can trigger their symptoms such as certain foods, medicines, emotional stress or anxiety - and treatment can involve changing diet and lifestyle to avoid these things.
If you notice that certain triggers affect your symptoms - such as fatty/spicy foods or stress - then you may want to consider ways to avoid these triggers.
Following a lowFODMAP diet has been found to help some people with IBS. However, it is a very restrictive diet which should only be done under the supervision of a trained dietician.
Bile acid malabsorption (BAM) can cause chronic diarrhoea. It is also known as bile acid diarrhoea or bile salt malabsorption. It can happen in people who have had an ileal resection for their Crohn's disease or have ileal inflammation. It can also occur if you have small intestinal bacterial overgrowth (SIBO), coeliac disease and chronic pancreatitis, among other reasons.
BAM can either be the result of your body producing too much bile acid (or bile salt) or it can be as a result of gastrointestinal disease - such as Crohn's disease.
In Crohn's disease BAM occurs when your ileum (the last part of your small intestines) is unable to absorb bile salt which is released by your body to digest food as it travels through your small intestine.
If you aren't able to absorb the bile salt then it moves into your colon. Your body then sends water to the colon and this causes diarrhoea.
There are a few medications available for bile acid malabsorption. These medications are not always effective for everyone. These include colestyramine and colesevelam. Some people use loperamide to manage it, but you should speak to your doctor about doing this.

If you have an unidentified food allergy or intolerance then this may cause you gastrointestinal issues.
Food allergies and food intolerances are two very different things. In a food allergy the body’s immune system reacts to a food. In general it is a mild reaction, but for some people it can be very serious. Symptoms of a food allergy include itching around mouth, ears or throat; itchy red patches; swelling in parts of the face and vomiting. In some cases people can have a severe allergic reaction (anaphylaxis). This can be fatal.
Food allergies tend to be life-long. If you think you have a food allergy then speak to your doctor.
A food intolerance happens when you have difficulty digesting a certain food and have unpleasant symptoms in reaction, usually a few hours after eating it. These may include bloating, stomach pain, diarrhoea, itching. The symptoms may come on more slowly than a food allergy.
Food intolerances may be a life-long issue or something that may resolve over time if other issues are the cause such as SIBO (see below).
There are various tests that can be done for food allergies and intolerances but they are not all accurate (particularly in the case of a food intolerance). If you think you have an intolerance keeping a food and symptom diary may help you identify which food/s it may be. Once you have an idea which foods may be causing you a problem you could try cutting them out from your diet one at a time for at least two weeks each. After this try reintroducing the food and see if your symptoms return.
If in any doubt speak to your doctor.
Some companies, such as Healthpath* (this is an affiliate link), provide home food sensitivity testing.
*Please note this is an affiliate link which means if you buy from the company we may receive a commission. You will pay the same price as you normally would and any money earned will be used to support IBDrelief's work.
Our guts are made up of trillions of bacteria. The majority of these bacteria live in our colon but sometimes some of the bacteria which should be living in your colon ends up in your small intestine1. This is known as small intestinal bacterial overgrowth - or SIBO. In a small number of cases SIBO occurs as a result of an overgrowth of the bacteria which are meant to be in your small intestine. This overgrowth can interfere with digestion of food and absorption of nutrients. This tends to happen by the bacteria damaging the cells lining the small bowel (the mucosa). Some people believe this damage can lead to leaky gut although not all medical professionals recognise this as a condition.
Symptoms of SIBO include bloating, abdominal distension, abdominal pain or discomfort, diarrhoea, fatty stools, fatigue, gas, belching, and weakness. In some severe cases weight loss and nutritional deficiencies may be present, particularly iron and vitamins A, B12, D, E and K. It can cause serious health issues if left untreated.
The believed cause of SIBO is complicated and may be as a result of a number of factors (or a combination of many). These can include:
It’s not known exactly how much of the population suffers from SIBO, though some studies suggest 6-15% of healthy people suffer and up to 80% of people with IBS2. Many doctors are also not aware of the condition or do not realise how common it is.
Diagnosing SIBO is difficult. Breath (hydrogen and methane) tests are the most common method but they aren’t completely accurate and can actually return false negatives. Another method is through culturing the bacteria from a sample taken from the small intestine, but to do this a long tube has to be inserted into the patient to retrieve a sample. Again, this method is not always accurate.
SIBO may be diagnosed just on your symptoms and your risk factors. Treatment can also be hard. The most common method is through taking antibiotics to kill off the bacteria, however SIBO often returns within a year (in up to a half of cases). Prolonged and repeated used of antibiotics is not recommended. Many doctors are now using a course of antibiotics alongside a probiotic with greater success. Some practitioners focus on treating the underlying cause of the SIBO by making changes to diet and lifestyle. This method can take time but is successful for many people.
It is possible to pay for a private SIBO test, such as this one from Healthpath* (this is an affiliate link).

It may sound made up but toilet anxiety is a real thing and it’s actually very common. It makes sense that people with IBD (and/or IBS) may develop anxiety when they are not in the vicinity of a toilet. Often this anxiety can cause stress on the body which actually makes things worse and can cause some gastrointestinal symptoms to happen. Your past experiences can also have an effect on your present thinking - for example if you’ve soiled yourself while on a bus before then you may become anxious about this happening on all future bus journeys - even if your IBD is in remission.
Talking therapies (such as counselling or CBT), hypnotherapy and relaxation therapies (such as meditation and mindfulness) help some people to overcome toilet anxiety.
A parasite is an organism that benefits at the expense of another. And, as uncomfortable as it is to think about, intestinal parasites are fairly common. They come in all shapes and sizes and live in different parts of our bodies. Intestinal parasites are those that live within the digestive system. Common intestinal parasites include:
The symptoms of an intestinal parasite can vary depending on the type you are carrying but may include digestive pain, gas, bloating, fatigue, anal itching, weight loss, changes in appetite, diarrhoea, vomiting, malnutrition.
Diagnosing a parasite infection may include looking for signs of a parasite around your anus or in your stools, having a stool test carried out or having blood tests done. If a tapeworm is suspected X-rays may be carried out. Comprehensive parasite stool tests can be done privately. This article includes more information about testing.
Treating a parasite infection can involve taking medication to kill the parasite.
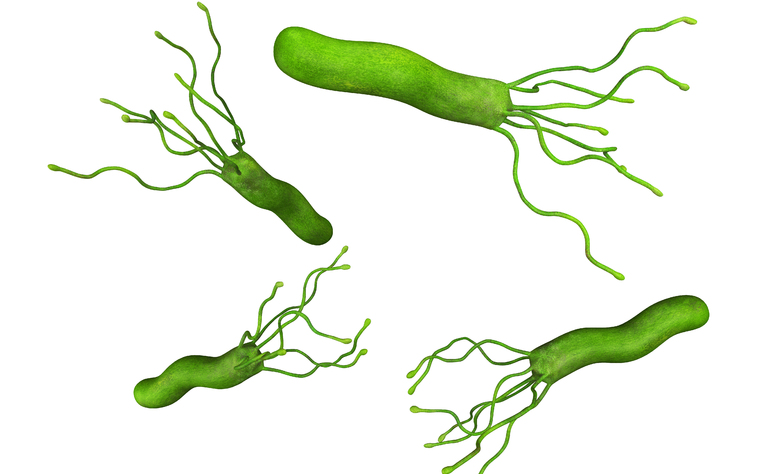
Gastritis is inflammation of the stomach lining. It usually occurs after the lining has been damaged from a bacterial infection. In some people it doesn’t cause any symptoms, but in others it can cause indigestion, gnawing or burning stomach pain, nausea, vomiting, feeling full after eating. Where the stomach lining has been worn away people with gastritis may also experience pain, bleeding or a stomach ulcer.
Gastritis may be caused a number of different things including:
Diagnosis of gastritis may involve a stool test, breath test for a Helicobacter pylori (H. pylori) infection, an endoscopy and/or barium x-ray.
Treating gastritis may depend on its cause. Some treatments include reducing acid in the stomach, treating H. pylori infection, and stopping the use of NSAIDs.
During their period many women also experience diarrhoea. It’s not known exactly why you experience diarrhoea during this time but it’s thought to be linked to prostaglandin which causes your bowels to contract during this time which can lead to loose stools, diarrhoea and stomach pain. Some women also experience bowel habit changes and other gastrointestinal symptoms (such as bloating and nausea) in the week before their period.
The best way to work out if your bowel issues are linked to your period is to track your symptoms alongside the dates of your period for several months. You may start to see a pattern emerge which will help you to predict when your symptoms are likely to be worse in the future.
*Please note this is an affiliate link which means if you buy from the company we may receive a commission. You will pay the same price as you normally would and any money earned will be used to support IBDrelief's work.
Jan Bures, Jiri Cyrany, Darina Kohoutova, Miroslav Förstl, Stanislav Rejchrt, Jaroslav Kvetina, Viktor Vorisek, and Marcela Kopacova; World J Gastroenterol. 2010 Jun 28; 16(24): 2978‐2990. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2890937/
Andrew C. Dukowicz, MD, Brian E. Lacy, PhD, MD and Gary M. Levine; Gastroenterol Hepatol (N Y) MD. 2007 Feb; 3(2): 112‐122. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3099351/



