A gastroscopy is used to look inside your digestive system via a camera inserted into your mouth.
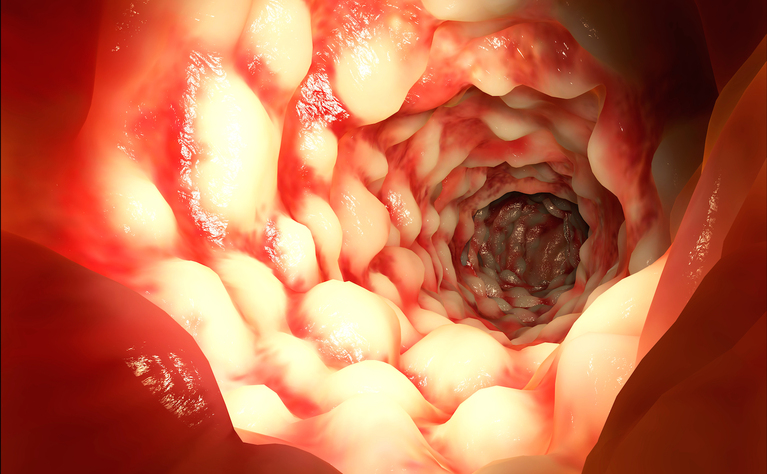
A gastroscopy - or upper gastrointestinal (GI) endoscopy - is a type of endoscopy in which a long flexible tube with a camera and light on the end is carefully inserted into your mouth and down your throat to look inside the oesophagus, stomach and beginning of the small intestine (duodenum).
If you have been experiencing gastrointestinal symptoms such as stomach pains, recurring indigestion or heartburn, vomiting and bloating or to monitor an ongoing condition.
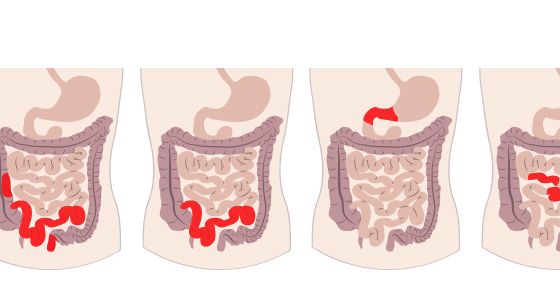
If you have suspected Crohn’s disease you may be given a gastroscopy to assist in diagnosis.
Upper gastrointestinal endoscopies are also used in the monitoring of diagnosed Crohn’s disease to check for inflammation.
Gastroscopies are usually carried out in hospital by a specially trained doctor or nurse. The procedure doesn’t take very long - often only 10-15 minutes. Most people will not need to stay in hospital overnight.
Before starting your throat will be sprayed with a local anaesthetic to numb it. You may also be given the option of a sedative which will make you drowsy and give reduced awareness about what’s happening.
When you are ready you will be asked to lie on your left side and a mouthpiece will be placed between your teeth. The end of the endoscopy will be placed into the back of your mouth and you will be asked to swallow. The tube will then be guided down your throat into your oesophagus and stomach. Air may be passed down the tube to help get a clearer view. The tube is thinner than your little finger and doesn’t get in the way of your breathing.
The camera transmits pictures on a screen in the room so that the doctor or nurse can see inside. Some biopsies may be taken to be examined.
You may find the gastroscopy procedure uncomfortable but it shouldn’t be painful.
Afterwards the doctor or nurse may discuss their findings with you or you may have to wait until the results of any biopsies are received, which can take several weeks.
If you’ve had local anaesthetic then you will likely be able to leave straight away, though you may not be able to eat or drink until your swallow reflex has returned, which can take around 45 minutes. If you’ve had a sedative then you will need to rest at the hospital for a couple of hours until that has worn off. It is wise to have someone collect you from the hospital and keep an eye on you for 24 hours afterwards until the effects of the sedative has passed.
You may feel a bit bloated afterwards but this should pass.
If you are having a gastroscopy because you have suspected Crohn’s disease then they will be looking for signs of Crohn’s disease, inflammation or causes of your symptoms.
If you have already been diagnosed with Crohn’s disease then the upper GI endoscopy will be used to monitor your condition and look for signs of inflammation.
A gastroscopy shouldn’t hurt but many people report finding it uncomfortable. Before the gastroscopy is carried out using anesthetic and/or sedatives to ease any discomfort will be discussed with you. It is normal to have nerves about the procedure, but if you are feeling particularly nervous or anxious discuss this with the nurse or doctor before.
Two weeks before your procedure you may be asked to stop taking any indigestion medication. Six to eight hours before you will be asked not to eat anything and stop drinking two to three hours before. This is to ensure the stomach is empty to allow a clear view of it.
The exact instructions will vary from hospital to hospital so you should follow any instructions you are given by them.
A gastroscopy is generally a very safe procedure. However, there are some risks. These include: