Name: Bernard Leach
Year of Birth 1947
Lives: Manchester, UK
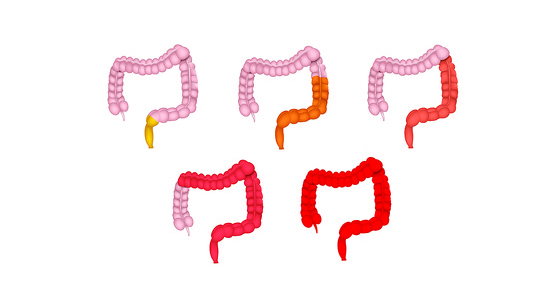
Type of IBD: Ulcerative colitis
Diagnosis Date: 2004
I first went to my GP with concerns about blood in my stools in early 2004. I had started to keep a health diary to keep a track of what was happening to me when I visited doctors. My inability to retain what doctors were telling me meant I started to make notes each time I had an appointment. Most doctors were happy with me doing this. I will go into some detail about my ‘career’ as an ulcerative colitis (UC) patient, because I know people in the IBDrelief community might be going through very similar things
Sometime later, in June 2004 I went for my first sigmoidoscopy at Wythenshawe hospital in Manchester. At an appointment with my GP after this I was told I had ulcerative colitis. He showed me the letter from the consultant which said: “In the distal sigmoid colon mucopurulent exudates was present. In addition there were multiple small ulcers Diagnosis: UC moderately active involving the recto sigmoid.” I was then put on Balsalazide tablets
This was followed by a second sigmoidoscopy in September 2004 which concluded: “In the rectum the mucosa was granular and congested. In the distal sigmoid colon the mucosa was granular and congested. The rest of the visualised bowel was normal. Diagnosis: UC mildly active involving the recto sigmoid”
A few words about me. I was born in 1947 and had polio when I was a baby which left me with very weak right leg and hip. I was a lecturer at Manchester Metropolitan University and retired five years ago. As far as I know there has been no interaction between the polio legacy and UC, but neither have made life easier
After the initial UC diagnosis, like many other people, I researched widely about the disease, went on many online forums, tried alternatives cures like VSL#3 probiotic. Considered some of the weirder ‘cures’ (faecal transplants, Palaeolithic diets etc.), went on an expert patient’s course and talked to my consultant (who has been consistently excellent).
By 2006 I was on 150gm Azathioprine per day - Balsalazide Sodium Capsules 9 x 750mg per day and Asacol mesalazine foam enemas but my symptoms seemed to be getting worse rather than better.
After a third sigmoidoscopy in 2009 the results were active recto sigmoid colitis. Distortion of glandular architecture. No dysplasia or malignancy. Active chronic proctocolitis. White blood cell count ‐ low, normal range. Expansion of the lamina propria (superficial layer). Mildly anaemic. Layers 1-5 OK; F-6 & G-7 showed active colitis
By then the Balsalazide was replaced with Asacol tablets (4.8gm per day), a higher dose of Azathioprine (200mg per day) and the dreaded Prednisolone - a steroidal anti-inflammatory drug (initially 10mg per day). I also had a bone densitometry scan (as bone density can be affected by steroids) which was just in the OK range, but told to take Calcichew D3 tablets as a supplement.

As things were not getting any better, and after a fourth flexible sigmoidoscopy in 2010, my consultant discussed the various options. He had been steadily putting me on heavier, more serious (ie with potential side effects) drugs and the options he gave included Mercaptopurine an immunosuppressive drug; Infliximab : a monoclonal antibody against TNFα used to treat autoimmune diseases; cyclosporine for steroid resistant colitis (intravenous then oral).
Also at this time Wythenshawe hospital appointed their first dedicated IBD nurse. This was a great step forward in that I was no longer reliant on the very infrequent appointments with the consultant and could contact the nurse independently. He suggested I join an IBD patient panel (which I did) and suggested a change in my diet, especially when flare ups occurred and go for a low residue diet (rice crispies, white bread, pasta, rice, fish, chicken, boiled pots, eggs, peas, soft carrots, no greens). There were also minor changes in my prescription drugs (enemas, suppositories, methotrexate, lomotil). I had a go at all these and added VSL#3 probiotic, which I had to get sent to me from Holland in cool bags.
By June 2010 I was getting desperate again - blood in stools and constant diarrhoea. I was having to go to the toilet an average of about 12 times per day. So I was put back on the Prednisolone (40mg per day, then tapered off over time).
Later that year, in October 2010, my consultant suggested it was time to consider using Infliximab, an anti-TNF (anti-tumour necrosis factor) drug. In order to see whether I could take this treatment I needed a chest X-ray and a series of blood tests). However, the chest X-ray showed pleural thickening of the apices (the rounded top portion of the lung). This needed to be checked out as Infliximab could exacerbate this. In December 2010 I went to see a chest doctor at the NW Lung Centre, Wythenshawe. I was then on two regular drugs - Azathioprine and Mesalazine - backed up with Salofalk liquid enemas, courses of prednisolone when I had flare ups and doses of lomotil to bung me up when travelling.
The blood and skin test for TB had both come back negative. The pleural thickening of the apices could be due to ‘old’ TB and the tests could be false negatives, but the chance was less than 5%. It could be something else ‘subtle and non-specific’ After a long discussion with the consultant over the risks involved with different strategies we agreed to go ahead with an Isoniazid straight away to treat any residual TB as there is a ‘small risk of a bad effect’ (TB activation) when you take Infliximab. The treatment would take 6 months, but it was agreed that I might be able to start on Infliximab after 2-3 months of treatment as the treatment should have got rid of any residual TB by then. There was a 5-10% chance of side effects ‐ inflamed liver, rashes, neuropathy (hands and feet), and hepatitis. These were monitored through monthly blood tests which looked at a full blood count, liver function and kidney function. Fortunately none of these side effects occurred and the only negative indicator was that whilst white blood cell count normal the lymphocyte was low on white blood cells. Haemoglobin count was also a bit low
Infliximab surgically targets and takes out part of the immune system. It prevents the formation of granulomas (a type of immunological response and signalling mechanism). It is taken by intravenous drip, followed by a 2nd one 2 weeks later, then one 4 weeks later, and then reviewed in clinic. Like all Monoclonal AntiBody drugs its name ends in MAB (or so I was told). It also cost in the region of £1,600 per shot, so thank goodness for the NHS. As anybody who consults online IBD forums, you really notice the difference between US & UK participants, with the former frequently complaining about the cost of the drugs they take for IBD.
Another flexible sigmoidoscopy in February 2011 showed that there was “inflammation in the first part of the bowel. Diverticulum was seen. Biopsies have been taken”.
After my bloods were finally OK I was called into the Programmed Investigations Unit (PIU) at Wythenshawe for my first infusion of Infliximab in March 2011. Over the next four months I had one infusion per month. Then from June 2011 onwards I was put on eight week cycle of infusions. Many blood tests later, and after a flexible sigmoidoscopy that showed some reduction in inflammation leaving behind some pseudo-polyps or false polyps which are a reaction to previous inflammation in the colon (these were snipped off), the consultant and I agreed to stop the infusions. From my side I was feeling much better and a bit guilty at the cost of the infusions to the NHS. My last one (the 12th) was in January 2013.
My feelings about the Infliximab infusions are very positive. My UC had improved significantly (fewer flare ups), though at the same time I had been making various lifestyle changes which I think have also been important (more of this later). At the time Infliximab had been used almost solely to treat Crohn’s disease and not UC. Oddly, I found the infusion sessions at the PIU to be very enjoyable. It was painless and being retired there was no pressure about the half day each infusion required. I got to know the staff well, talked to several other day patients, got to listen to audiobooks on my phone and enjoyed the NHS lunches and cups of tea.
Lifestyle changes
On reflection, I think I felt that if the NHS was willing to make such an investment in my treatment that I should play my part and make some positive changes to my lifestyle. In August 2012 I watched Michael Mosley’s programme for BBC Horizon called Eat, Fast & Live Longer. In this he investigated the benefits of intermittent fasting. He then went on to write about the 5:2 diet (ie 2 days fasting per week) though he initially investigated alternate day fasting (ADF). I was very impressed with the programme and decided to give ADF a go. Over a period of a year or so I reduced my weight from 13st 5lbs to 11st and as time went on I relaxed the regime to alternate eating days with ‘not eating a lot’ days rather than ‘non eating days’ (or change from ED & NED to ED & NEAL!). At the same time I improved my diet so that on NEAL days I now have salads and fruit salads, and some nuts (as a treat). On ED days I have these plus some cooked food (very little meat), bread and treats (like an occasional glass of red wine).
My view was that the initial non-eating days gave my bowels a rest and time for inflammation to perhaps heal. I discussed this with my consultant who said that there was not much evidence for IBD of bowel rest having such beneficial effects and there was a danger when you follow a very low calorie diet, that you lose muscle as well as fat so lower metabolic rate (the energy you expend over a day just keeping your body functioning ). Well, it seemed to work for me and I have continued with the alternate day habit, but not as rigorously as I did at the beginning.
At the same time as I changed my diet I also started to look at my fitness and in January 2013 was referred to a fitness adviser at my local health centre who put me on an NHS subsidised fitness course of gym circuit work-outs at Moss Side Leisure Centre. This was the first time I had ever set foot in a gym (age 66) and felt a little intimidated at first, but once the course was finished I decided to go to the gym on a regular basis. I have combined this with swimming and now most mornings I go for a 2km swim followed by 45 mins or so resistance training (weights machines) in the gym, which sets me up for the rest of the day.
Conclusions
We all know there is no miracle cure for IBD (UC in my case) and we have to tackle it in our own way ‐ getting advice, seeking treatments, trying alternative therapies, doing lots of research. I don’t think that what has worked for me will necessarily work for others. I have also been fortunate in not having had an extreme form of the disease. In my case my search has taken me through a dozen or more medicines (of which I disliked the steroids the most), online forums, expert patient groups, an IBD patient panel, various consultants and IBD nurses, TV programmes and fitness advisers
I have been without symptoms for nearly two years now. I wouldn’t say I am entirely normal, but bowel movements are only 2-3 times per day, with no urgency and no flare ups. I think that Infliximab, diet and exercise have all contributed to this - but it could just be luck. At one time I felt my UC was on an unstoppable spiral of flare ups and successively more powerful drugs seemed to be having little effect. At that point my consultant made a remark which really lifted me ‐ “You know, I have had patients with IBD in a similar position to you in which IBD was really disrupting their lives, when all of a sudden, things got better, for no apparent reason”.
So, whether it is just coincidence or not, I am just pleased at the disappearance (for now) of my symptoms and that I can get on with my life without being tied to toilets.
Last week (19-10-15) I had my latest sigmoidoscopy at Wythenshawe Hospital “to assess mucosa prior to stopping azathioprine”. They found no inflammation, just some scarring where there had been previous inflammation. The doctor concluded that I could safely come off Azathioprine, but should continue with Mezavant. I stopped taking Azathioprine the same day.
My personal case study of having ulcerative colitis was written two year ago in October 2015. I had just had a sigmoidoscopy at Manchester’s Wythenshawe Hospital and it looked like there was no inflammation, just some scarring where there had been previous inflammation.
So I took this as a go-ahead to stop taking azathioprine and reduce my mesalazine from 3 to 2 then 1 tablet a day. So everything appeared to be going well. I felt like I had won my battles against UC! At the same time though I became less organised in what I ate and gradually left behind my previous diet. This meant I gradually put on some weight ‐ not a lot, about half a stone ‐ and I felt it was OK for me to eat and drink almost anything I wanted to.
Then in October 2016 symptoms of UC started to appear, gradually getting worse - blood & mucous in stools, urgency, toilet about 8x per day. I upped my mesalazine tablets to 2 per day. After contacting the IBD helpline the nurse suggested I start taking 4x 1200mg mesalazine tables per day and use a Salofalk 2gm liquid enema each night for 4 weeks to tackle the flare up. This largely did bring it under control.
In January I saw the IBD consultant. The blood test results were all satisfactory, so no sign of inflammation. After discussing all the options I agreed to go on predfoam (steroid enemas) ‐ 1 per night for 2 weeks, then 1 alternate nights for 4 weeks and up my azathioprine to 3 tablets per day. In May this year I had a colonoscopy which showed very mild inflammation in the rectum and lower sigmoid colonoscopy, By then I was feeling fine and back to normal, so I am now back to a maintenance dosage of azathioprine (2x 50mg daily) and Mesalazine (2x 1200mg daily).
Today I am feeling fine and more or less symptom free. The whole episode reminded me of the need to be careful of thinking you have ‘beaten’ IBD. You have to remain vigilant and keep to those behaviours which helped get rid of flare ups in the first place.
It is 19 years since I was first diagnosed with ulcerative colitis. It was seven years ago that I wrote about my IBD story for this website. It took me a long while to come to terms with my condition. At one point I felt that nothing I tried seemed to make any difference. I remember talking to my consultant about this at the time and he made a comment which has stuck with me since then. He said that he had many patients where nothing had seemed to work who then found that somehow, the IBD had just cleared itself. The lesson was to not give up hope.
I came to realise that I had to do something drastic about my diet to really tackle the problem. So for a start, I cut out bread, even though I'd always loved it. I then started to try fasting in order to give my bowels some rest. Discussing this with my consultant he thought it was a good idea though the evidence of it working was not yet proven. Well it did work for me then and it continues to do so.
At the beginning of the pandemic I was still on azathioprine, but only on a small dose. Because I was taking an immunosuppressant drug, I was placed in the category of vulnerable people who were advised to shield. As all my symptoms of ulcerative colitis had disappeared for quite a while, I stopped taking azathioprine all together in 2020 and since then I have been on no medication and have had no symptoms at all. I have continued with regular fasting and try to follow a healthy diet (not always successfully) to keep my weight down as well as to keep UC at bay. To be more specific my bowel movements are regular (once or twice a day), no sloppy stools or diarrhoea. It is easy to then think that you have overcome IBD forever and then to eat more of the foods that are likely to cause trouble, such as bread. I try to remind myself that I have IBD for life and am not permanently ‘cured’ and so far I have remained vigilant in sticking to my diet and fasting regime.