Find this article useful?
Why not sign up to our mailing list and receive regular articles and tips about IBD to your inbox.
Fistulas are a common complication of Crohn’s disease (approximately one third of people with Crohn’s disease will develop a fistula). They are less common with ulcerative colitis.
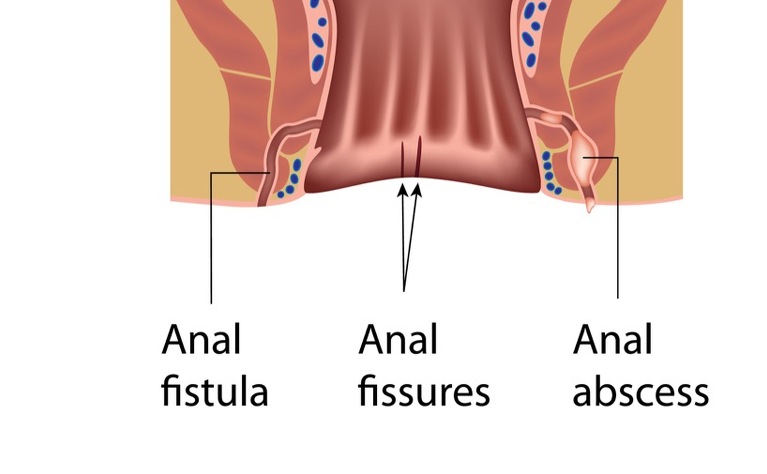
Fistulas are like tunnels which can form and connect either two different parts of the bowel together or the bowel to other organs - such as the bladder, vagina or skin. The most common site that fistula form is in the tissue surrounding the anus.
There are several different types of fistulas. These include:
About one in three people with Crohn’s disease will probably develop a fistula at some time and the longer you have Crohn’s disease the more likely you are to develop a fistula. Fistulas are much less common in people with ulcerative colitis (UC). This is because the inflammation in Crohn’s disease tends to penetrate the whole thickness of the bowel wall. This creates ulcers, leaks and abscesses and as they develop a hole can start to form which then becomes a tunnel creating a fistula. The inflammation in UC doesn’t penetrate through the bowel wall in the same way.
Small fistulas may not cause any symptoms but larger ones can become infected, causing complications. This can cause a high temperature. Other symptoms vary depending on where the fistula is. They include:
It is also common to develop an abscess at the site of the fistula.
If your doctor suspects a fistula then they will examine your skin to see if there is a fistula visible. If one if found then they may press on the area to see if pus or faeces leaks from it. If there is no obvious fistula then you may have some tests carried out. These include:
The treatment provided will depend on the type of fistula you have and the treatment you are already receiving for your IBD. Many fistulas close following treatment and do not return. Unfortunately the treatments for fistulas aren’t always successful and you may need several treatments before the fistula heals.
Some common treatments include:
Why not sign up to our mailing list and receive regular articles and tips about IBD to your inbox?