Have you ever wondered how a decision is made about what medication you should be given and when? This article takes a look.
Over recent years there has been a huge growth in the number of options available for treating inflammatory bowel disease (IBD), particularly in the area of biologic medications.
Great news for patients who now have a wider range of medicines available to help them get well. But with all these extra options available, how are decisions made about which treatment to give you and when?
To assist with this clinicians have a set of guidelines to help them figure it out.
These guidelines are known as patient treatment pathways. They set out different stages of a patient’s journey with a disease (in your case IBD) and the national recommendations to follow. In the UK local versions of these pathways are then created across different NHS areas. As well as taking into account the national guidelines the local versions highlight any local policies clinicians must follow.
These pathways set out a plan of what a patient should expect from their treatment, assists doctors in making decisions on what medication they give you and helps to ensure patients across different areas are receiving the same level of care.
They are based around the latest available evidence and balanced alongside financial costs of the different treatments. They are drawn up in consultation with clinical experts in the field.
When following these treatment pathways for IBD your gastroenterologist will need to take into account several things before a decision can be made1. These include:
In the UK the National Institute of Clinical Excellence (NICE) sets out national pathways. View the pathways for:
The pathways follow the full journey for a patient, from when IBD is first suspected, right through to when their disease is in remission and how they are monitored.
A large part of the pathways focus on treatments to induce remission (get you well) and maintain remission (keep you well). These guidelines follow a traditional treatment pathway of ‘step-up’ therapy for mild to moderate cases of IBD.
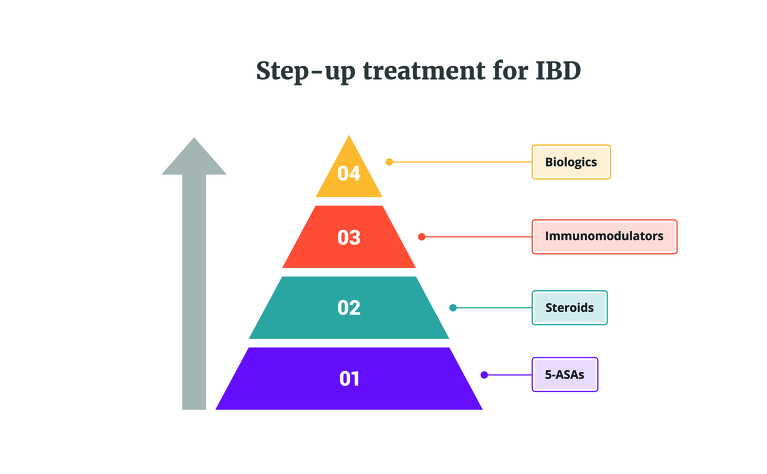
‘Step-up’ treatment essentially takes you through a ‘therapeutic pyramid’ of medications with four levels (2). In this approach you start at the bottom of the pyramid (tier 1 or 2) and if the medicines at this level don’t improve your symptoms then you ‘step-up’ a level to the next medications and so on, until you find a medication you can stay on long-term to keep you well.
The four tiers of the ‘step-up’ approach are:
Tier 1: 5-ASAs (e.g. mesalazine, sulfasalazine) - generally for ulcerative colitis only
Tier 2: Steroids (e.g. prednisolone, budesonide)
Tier 3: Immunomodulators (e.g. azathioprine, mercaptopurine, methotrexate)
Tier 4: Biologics (e.g. adalimumab, stelara, infliximab)
At each of these tiers there are more than one type of medication available and/or different preparations of the medication which you may be asked to try before moving onto the next tier. You may also be prescribed a medication from two different tiers to take at the same time (combination therapy). Typically, if you reach tier 4 and don’t respond to the medications in this tier then you may be considered for surgery to remove parts of your bowels.
The tiers have been created using “relatively safe medications, but with lesser efficacy, before incrementally increasing to medications of greater efficacy but potentially greater risk”2.
For those classified with severe disease the treatment you receive may look a bit different. If you are in hospital then you will be constantly monitored for signs that you may need surgery (particularly in those with ulcerative colitis) and you may receive biologic medications much earlier than those who are considered to have mild or moderate disease.
For patients who struggle to find a medication that puts/keeps them in remission it can mean a long process (sometimes over a year) of working through the different tiers before finding an effective treatment.
So, why don’t they just start at the top of the pyramid? Well, there are some researchers who are looking at whether a ‘top-down’ approach would be more suitable for some or all patients, and there are some doctors who have chosen to already work in this way. But, there are a few reasons why this isn’t the norm.
A blanket top-down approach seems unlikely, with cost being a huge factor. It’s widely known that prescribing clinicians are asked to choose cheaper medications to save money, where possible and appropriate. If patients were placed on the more expensive biologic treatments first the economic burden of IBD on healthcare systems would increase dramatically, which would be potentially unsustainable.
However, one thing that is changing this is the growth of biosimilars, cheaper copies of biologic medicines that are now coming to the market and reducing the cost and increasing access to this class of medication. In patients who are already taking biological medications the NHS says “switching patients from the original biological medicine to a biosimilar could save the NHS hundreds of millions of pounds”4.
Instead of a one-size fits all approach, there is certainly an appetite from both patients and clinicians to see a more personalised approach to treatment. A paper in the Journal of Crohn’s & Colitis in 2018 noted that: “clinicians yearn for a time when biomarkers will allow for treatment decisions in a ‘personalised’ or ‘precision’ medicine approach. This ideally should provide some guidance as to who will benefit from more intensive early therapy”5.
In the UK a biomarker prognostic test to predict if you are at risk of an aggressive disease course is now available to pay for privately. It’s currently being trialled to test accuracy in big groups of patients and going through a process to see if it can be provided on the NHS.
If approval is received then doctors may soon be able to more widely predict with greater accuracy the likely severity of a person’s IBD and use a treatment more appropriate for them earlier. The hope with this is that patients will receive the right treatment for them, at the right time - saving a lot of stress and money for both patients and doctors.